Spinal stenosis - treatment and surgery
Spinal conditions can seriously reduce a patient's quality of life, leading to problems with self-care, chronic pain, and limited mobility. One such condition is spinal stenosis, a narrowing of the spinal column that compresses the nerves.
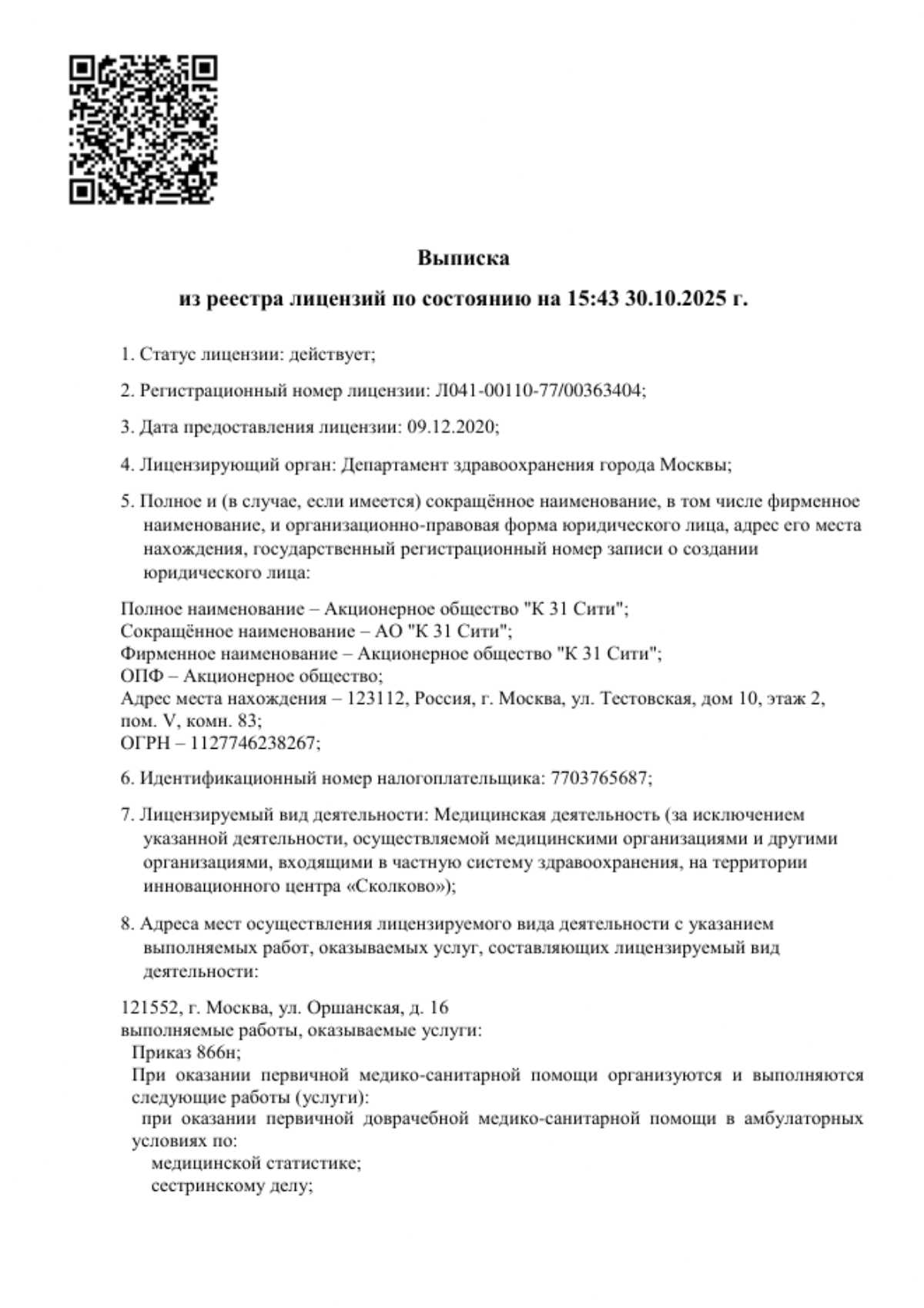
At the K+31 Medical Center, we diagnose and treat spinal stenosis: specialists use both conservative and surgical methods.

specialists

equipment

treatment
Classification of stenosis
Depending on the location, the pathology can be central or develop in the lateral portion. In the former case, the anterior region of the spinal column narrows. In the latter case, small openings develop between the vertebrae. There is also a classification based on the severity of development.
Absolute stenosis
This is a dangerous condition in which the narrowing reaches critical levels. The cavity size after compression does not exceed 10 mm. The pathology is characterized by complete loss of sensation, severe motor impairment, and leads to disability.
Relative stenosis
This is the initial stage of the disease, with a narrowing of less than 12 mm. A person experiences weakness in the legs, numbness in the extremities, and back pain. If the nerve roots are damaged, the pain becomes severe and decreases in intensity when bending.
If the condition is left untreated, myelopathy—a degenerative process in the spine—develops.

Causes and risk factors
The pathology can be congenital or acquired during life. The primary form develops as early as the third week of pregnancy. The cause is a genetic predisposition. Stenosis can develop as a result of infection or exposure of the fetus to toxic substances.
The secondary, acquired form develops for reasons such as:
- Trauma to the vertebrae, hematomas within the canal
- Degenerative changes, degenerative processes in the joints, in which bone tissue penetrates the spinal canal
- Herniated disc with subsequent ossification
- Displacement of vertebrae due to anatomical imbalances in the spinal arch
- Thickening of the vertebral ligaments due to inflammation and degeneration
- Thickening of the joint capsule between the vertebrae due to inflammation is a common symptom of Bechterew's disease
- Disturbances in the structure of the longitudinal ligaments
- Congestion of the veins
- The appearance of scars in the spinal canal is often observed during surgical procedures where metal elements are inserted into the spine.
- Tumors, cystic formations
The development of stenosis is the result of both congenital and acquired factors. Elderly patients are most susceptible to the disease due to degenerative processes that occur with age.
A predisposing factor for the acquired form is advanced osteochondrosis, with bone overgrowth and the appearance of osteophytes.

Symptoms of spinal stenosis
Symptoms progress slowly, and the disease can take years to develop. When the lumbar or thoracic region is affected, the patient complains of gradually increasing discomfort in the lower extremities and back. Initially, the pain occurs only with movement.
The discomfort is not clearly localized; most patients describe it as a diffuse, unpleasant sensation. While walking, weakness in the legs—a neurogenic limp—appears. The person constantly wants to stop, sit, or lie down. The discomfort decreases with bending the knees and leaning forward. Patients with spinal stenosis do not complain of pain even when driving for long periods.
Over time, sensory disturbances develop—numbness in the legs, goosebumps. Symptoms of the disease may be limited to one or both sides. As the disease progresses, pelvic dysfunction occurs—difficulty with defecation, urinary incontinence, and, in men, erectile dysfunction. With prolonged damage to the lumbar nerves, muscle mass in the legs is lost. Damage to the chest area manifests as spasticity in the legs.
Cervical damage often has no specific signs. Symptoms appear in the late stages. A characteristic symptom is intense pain in the neck, radiating to the shoulder blades and arms. The patient complains of spasms that intensify with head movements. The arms become weak and tingling. The legs become weak, the person has difficulty walking, and constantly stumbles. Associated symptoms include constipation and urinary problems. With damage to the 3rd and 4th cervical vertebrae, respiratory function is impaired, and spasticity appears in the upper and lower extremities.

Diagnostics of stenosis
If any complaints arise, you should consult an orthopedist for a timely diagnosis. During the examination, the doctor checks neurological reflexes, reviews the patient's medical history, and clarifies information about injuries.
Here are the main examination methods:
- MRI. These images show the structure of discs, joints, and the characteristics of nerve fibers. This method helps determine the extent of the disease and assess the condition of the spinal cord.
- CT scan. Using this image, the doctor examines the structure of bone tissue, identifying osteophytes, their size, and the parameters of the foramen. CT scans can reveal herniated discs and hypertrophy of the vertebral arches.
- Myelography. This is a tomography scan with the introduction of a contrast agent. This method helps determine the degree of nerve root compression.
- Electroneuromyography. The procedure assesses the general condition of the nervous system and the contractile characteristics of muscle tissue. By recording electrical impulses, it is possible to identify transmission disturbances and diagnose the nature of neurological abnormalities.
It is important to differentiate stenosis from respiratory diseases and angina. In some cases, the patient requires consultation with a pulmonologist or cardiologist.
Treatment of stenosis
Lumbar spinal stenosis is treated conservatively or surgically. Let's take a closer look at each method.
Conservative treatment
In most cases, the condition can be improved with medication. For this purpose, the doctor prescribes nonsteroidal anti-inflammatory drugs. They relieve pain and reduce swelling. They should be taken under the supervision of a specialist and in a strictly defined course.
If the cause is an infectious agent, the treatment plan includes antibacterial medications. Urinary disorders and swelling require diuretics.
To improve nervous system function and regenerate damaged fibers, B vitamins are indicated, most often in injection form. To relieve muscle spasms and reduce discomfort, muscle relaxants are prescribed—in tablets or injections.
Conservative methods include physiotherapy. Electrophoresis delivers medications to the affected areas using electrical impulses. Magnetic therapy relieves inflammation and discomfort. Physical therapy increases range of motion, strengthens muscle tissue, and helps maintain joint flexibility. To reduce inflammation, your doctor may recommend therapeutic mud treatments and balneotherapy (baths).
Important: manual therapy is not recommended at any stage of lumbar spinal stenosis, as it can lead to complications!
Surgical treatment
If medications are ineffective, the orthopedist will refer the patient for surgery, which is performed by a neurosurgeon. 95% of surgical interventions are elective. The goal of this procedure is to reduce or completely eliminate the impact on the nerve endings and the spinal foramen. The following techniques are used for this purpose:
- Removal of a section of the adjacent vertebra
- Resection of the joint between the vertebrae
- Removal of a section of the spinous process in the affected area
- Foramen widening
These methods can be combined. The method is selected individually, depending on the patient's condition and the specific clinical circumstances.
Indications and contraindications for surgery
The primary indication is the ineffectiveness of conservative treatments. If pain intensifies, sensitivity decreases, and the patient develops spasticity—increased muscle tone with abnormal tension in the limbs—the doctor recommends surgery. Surgical treatment is used for bowel and urinary disorders.
Microsurgery is often used for decompression, with incisions no larger than 3 cm and a surgical microscope used for precision. This approach ensures safety and rapid recovery. Before surgery, surgeons ensure there are no contraindications. These include:
- Advanced-stage comorbidities – severe heart failure, respiratory failure
- Acute infectious processes
- Malignant neoplasms with metastasis
- Absence of pronounced symptoms – surgery is indicated only for severe neurological disorders
Before surgery, the patient consults with an anesthesiologist, undergoes blood and urine tests for possible infectious agents, and undergoes an ECG to assess cardiac function.
FAQ
Which doctor treats spinal stenosis?
Conservative treatment is prescribed and monitored by an orthopedist. If neurological disorders are present, the patient consults with a neurologist. Surgery is performed by a neurosurgeon, and the patient is monitored by a rehabilitation specialist during recovery.
Is it possible to cure spinal stenosis?
This condition can go into remission if the primary goal—relieving compression of the nerve fibers—is achieved. Conservative treatment cannot eliminate the problem, but if therapy is started promptly, medications can eliminate inflammation, pain, and swelling and can improve a person's well-being for years.
How can I prevent the development of this pathology?
Follow preventative measures. Avoid excessive physical activity. Monitor and manage your weight promptly: obesity is a predisposing factor. If you engage in heavy physical labor or professional sports, try to prevent spinal injuries. Treat bone and joint pathologies promptly.

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price
Other services







































































What is spinal stenosis?
This is a pathological condition in which the spinal cavity narrows. This occurs in the central and lateral areas, near the intervertebral foramina.
Stenosis occurs due to compression of nerve endings by soft tissue and bony spurs penetrating into the empty cavity. This results in pressure on the spinal cord and spinal nerve fibers, and the patient experiences characteristic symptoms—severe pain and loss of sensation.
The location of the pain depends on the location of the lesion. Symptoms most often develop in the lumbar region.