Epithelial Pilonidal Tract: Treatment, Removal (Excision) Surgery
The epithelial pillow (EPT) is a narrow tube whose walls are lined with cutaneous epithelium containing hair follicles, sebaceous glands, and sweat glands. This rudimentary canal has one or more pinpoint openings on the skin's surface. Over time, its cavity accumulates waste products from the glands, lost hair, and dead skin cells, creating ideal conditions for infection and inflammation.

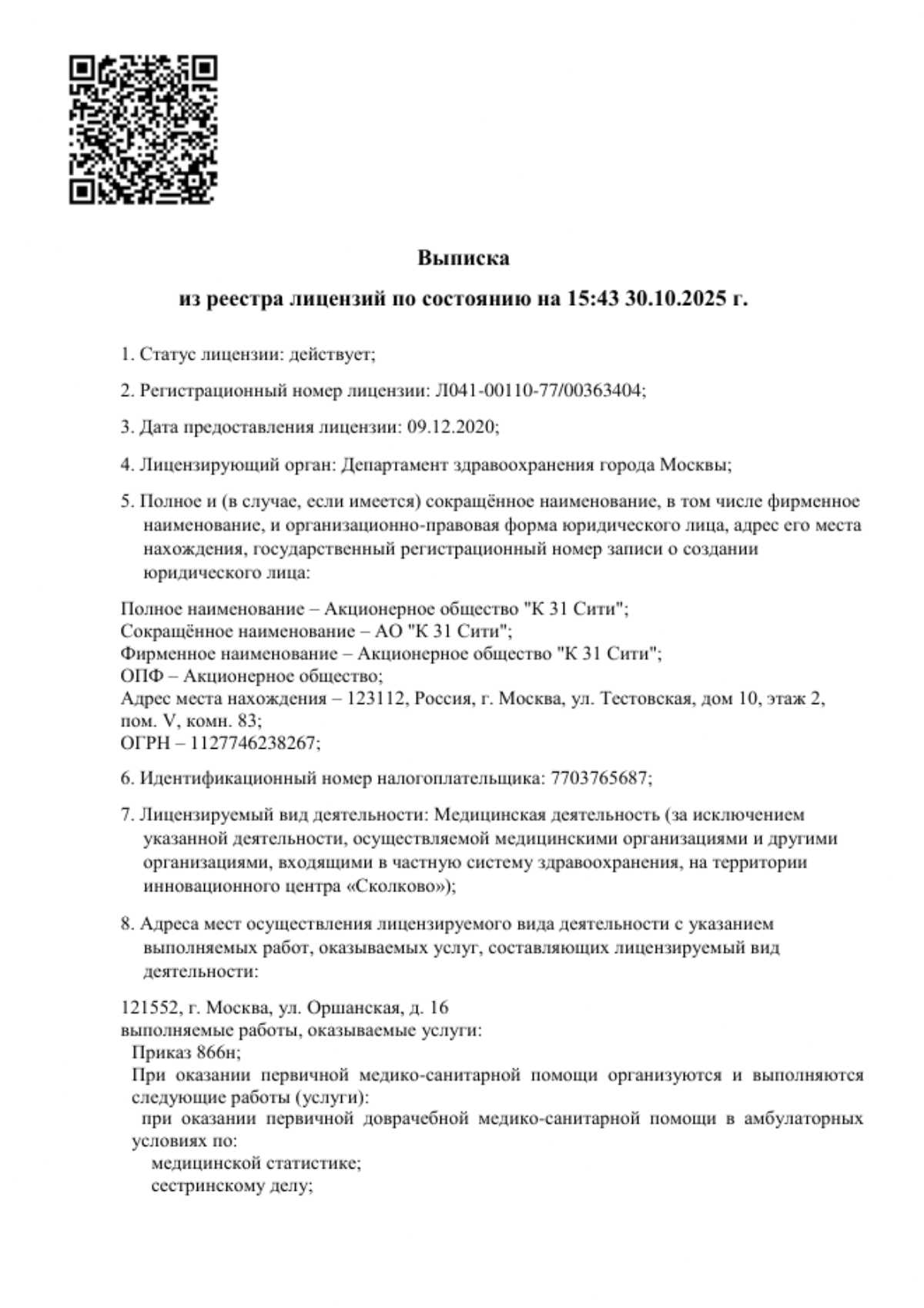
specialists

equipment

treatment

Symptoms and complications
The clinical presentation of the disease directly depends on the stage: whether the canal is dormant or has entered a phase of active inflammation. Each symptom is an important signal that a qualified physician should pay attention to in order to provide timely assistance.
Clinical presentation of epithelial coccygeal tract
In the uncomplicated stage of epithelial coccygeal tract, there is no inflammatory process. The disease may be asymptomatic, manifesting only by the presence of one or more small fistula openings in the intergluteal fold. As inflammation develops, characteristic clinical manifestations arise that require specialist attention:
- Pain in the coccyx area, usually aching or nagging, intensifying with sitting, walking, and physical activity.
- Appearance of a painful infiltrate (hardening) with a local increase in skin temperature and pronounced edema.
- Hyperemia of the skin over the area of inflammation.
- Purulent or serous (bloody) contents may be released from fistula openings.
- With the formation of an acute abscess, systemic symptoms are possible: fever, chills, general weakness, and malaise.
Complications and consequences
The process is not limited to superficial inflammation. The infection quickly spreads deeper, destroying surrounding structures. Ignoring the problem or attempting self-treatment is unacceptable, as this directly leads to the development of serious complications. If left untreated, the disease inevitably becomes chronic, which can lead to the following consequences:

-
Recurrent abscess. An established abscess may spontaneously burst, bringing temporary relief. However, without addressing the underlying cause (the abscess itself), the abscess will continue to form again and again.
-
Secondary fistulas. Pus seeks an outlet and can form new pathological tracts that open into the skin of the buttocks, perineum, or even the scrotum. This significantly complicates subsequent surgical intervention.
-
Spread of infection. Inflammation can spread to surrounding fatty tissue, causing phlegmon – a diffuse purulent inflammation that is life-threatening.
-
Squamous cell carcinoma. In extremely rare cases, a long-standing, recurring chronic inflammatory process can lead to malignant cell transformation.
Diagnostics
Establishing an accurate diagnosis is the key step in determining the appropriate treatment strategy. At our clinic, diagnosing sacrococcygeal sinusitis is performed by experienced surgeons and is usually straightforward.
Clinical Examination
The basis of diagnosis is a thorough medical examination. The surgeon examines the sacrococcygeal region, identifying the primary openings of the tract, assessing the skin condition, and the presence of indurations. Palpation (feeling) allows one to determine the location and size of the inflammatory infiltrate.
Instrumental Diagnostics
In most cases, a clinical examination is sufficient. However, in cases of complex, branched tract systems or suspected purulent drainage, additional tests may be required, such as fistula probing, soft tissue ultrasound, or MRI for detailed visualization of the pathological process.
Differential Diagnosis
It is crucial to distinguish epithelial coccygeal tract from other conditions with similar symptoms in order to prescribe the correct treatment. The doctor must rule out rectal fistula, pelvic osteomyelitis, furuncle, carbuncle, and cystic lesions (teratomas).
Causes and risk factors
Understanding the causes and risk factors helps in both treatment and prevention of exacerbations.
Causes of occurrence
The main reason the disease transitions from a dormant to an active stage is blockage of the ducts. This leads to stagnation of secretions, infection, and, as a result, the formation of a painful purulent lesion—an abscess. Without adequate treatment, the process can become chronic with periodic exacerbations.
Risk factors
There are a number of conditions that significantly increase the likelihood of pilonidal cyst inflammation. The presence of one or more of these is a reason to consult a doctor.
- Excessive hair growth in the sacrococcygeal region
- A sedentary lifestyle, occupations that involve prolonged sitting (drivers, office workers)
- Poor hygiene of the intergluteal fold
- Excessive sweating (hyperhidrosis)
- Trauma and bruises to the coccygeal region
- Wearing tight, chafing underwear and clothing
- A weakened immune system
Epidemiology and pathogenesis
The disease is most often diagnosed in men aged 15-30, although it also occurs in women. The main theory behind its pathogenesis is the abnormal implantation of hair under the skin, which triggers an inflammatory reaction. Obstruction of the primary openings of the tract impairs the outflow of contents, which triggers the development of an acute or chronic inflammatory process.
Treatment methods
Conservative treatment
Conservative therapy is unable to remove the epithelium lining the pathological canal, and therefore does not address the underlying cause of the disease. This approach is aimed solely at combating inflammation and may include:
- Systemic antibiotics to suppress bacterial infection
- Using topical anti-inflammatory and antibacterial ointments
- Thorough hygiene of the sacrococcygeal region
This method is used either at the earliest stage of the inflammatory process or as preparation for a planned surgery after drainage of an acute abscess. It is important to understand that without surgical treatment, a new exacerbation is only a matter of time.
Surgical treatment
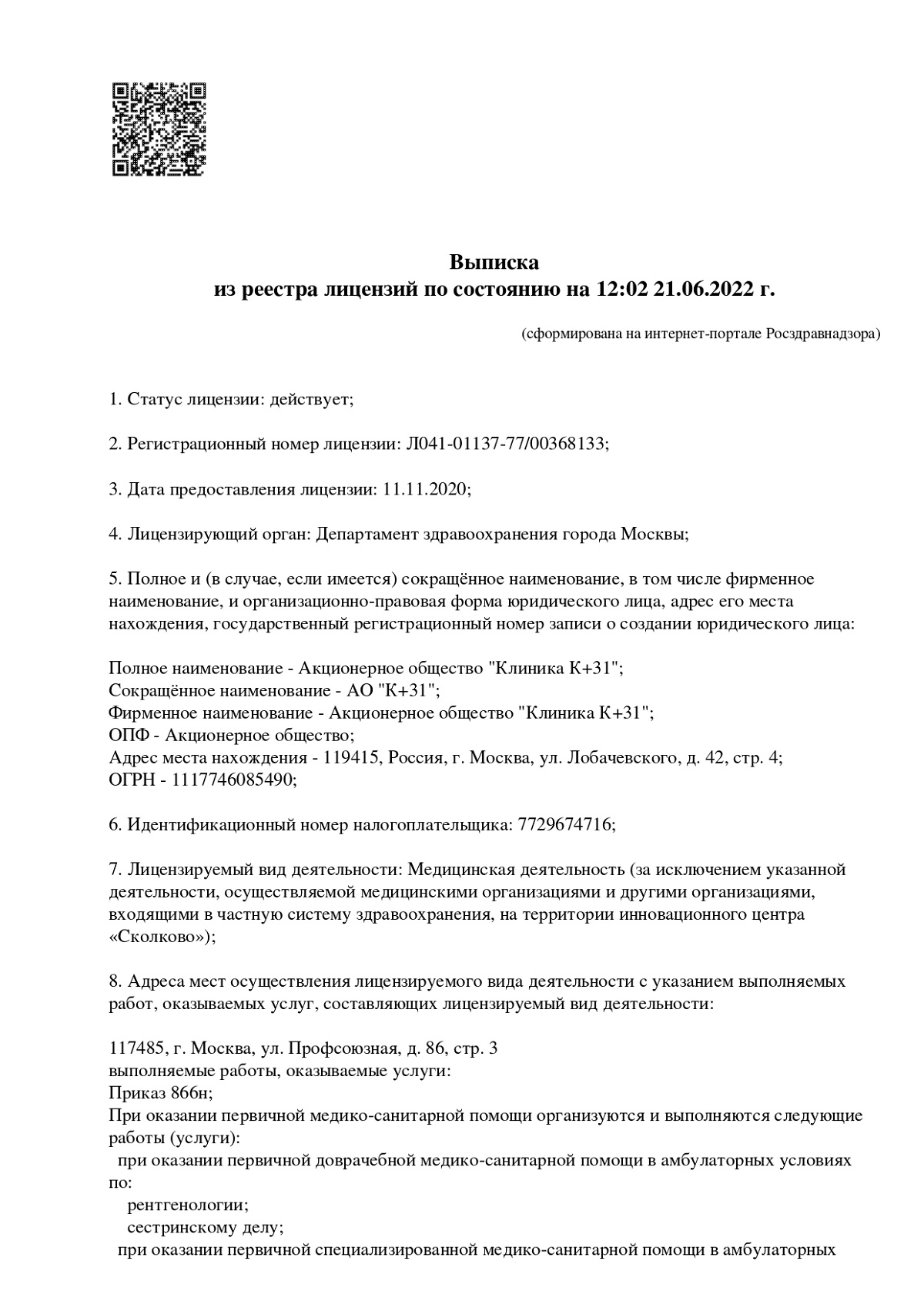
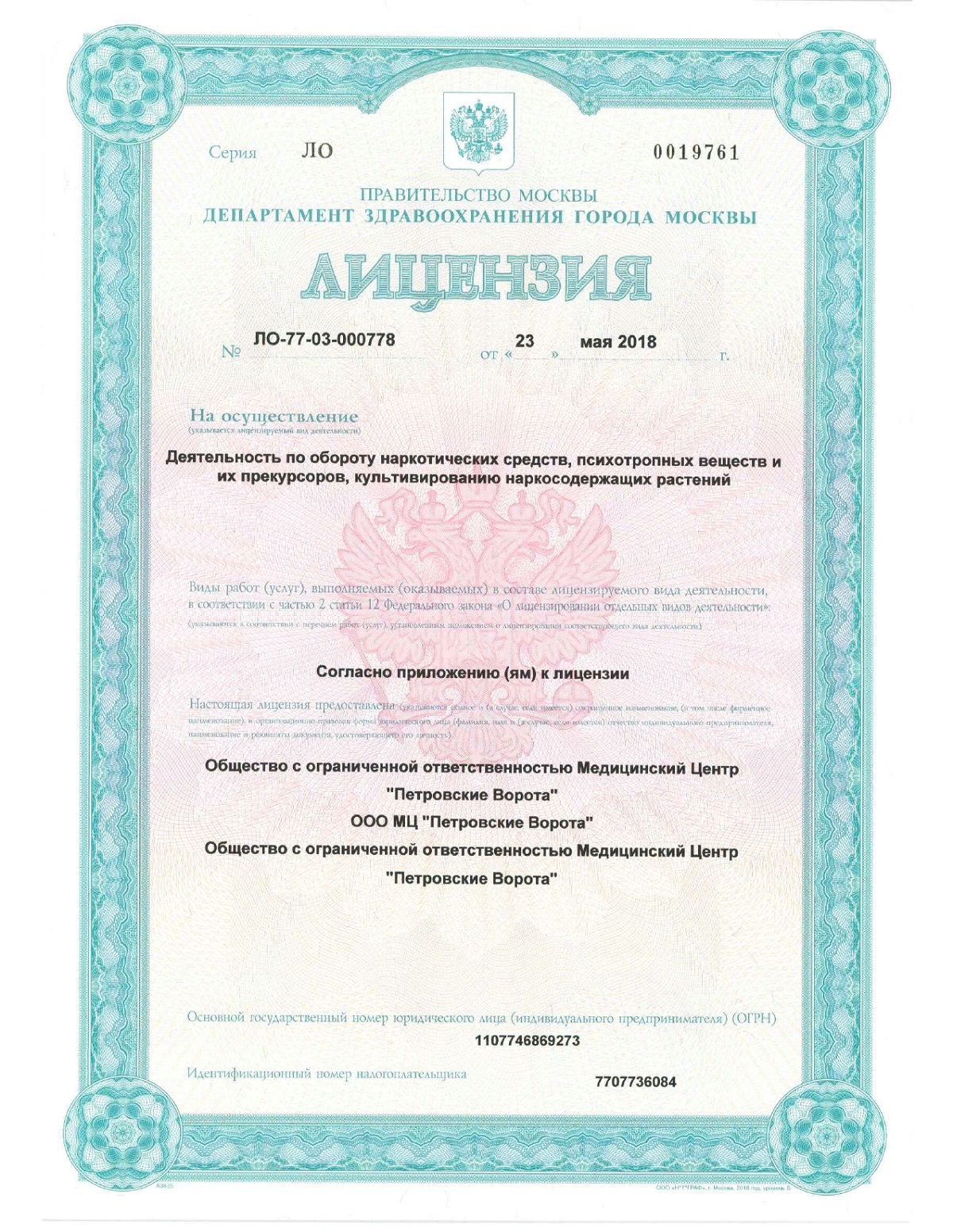
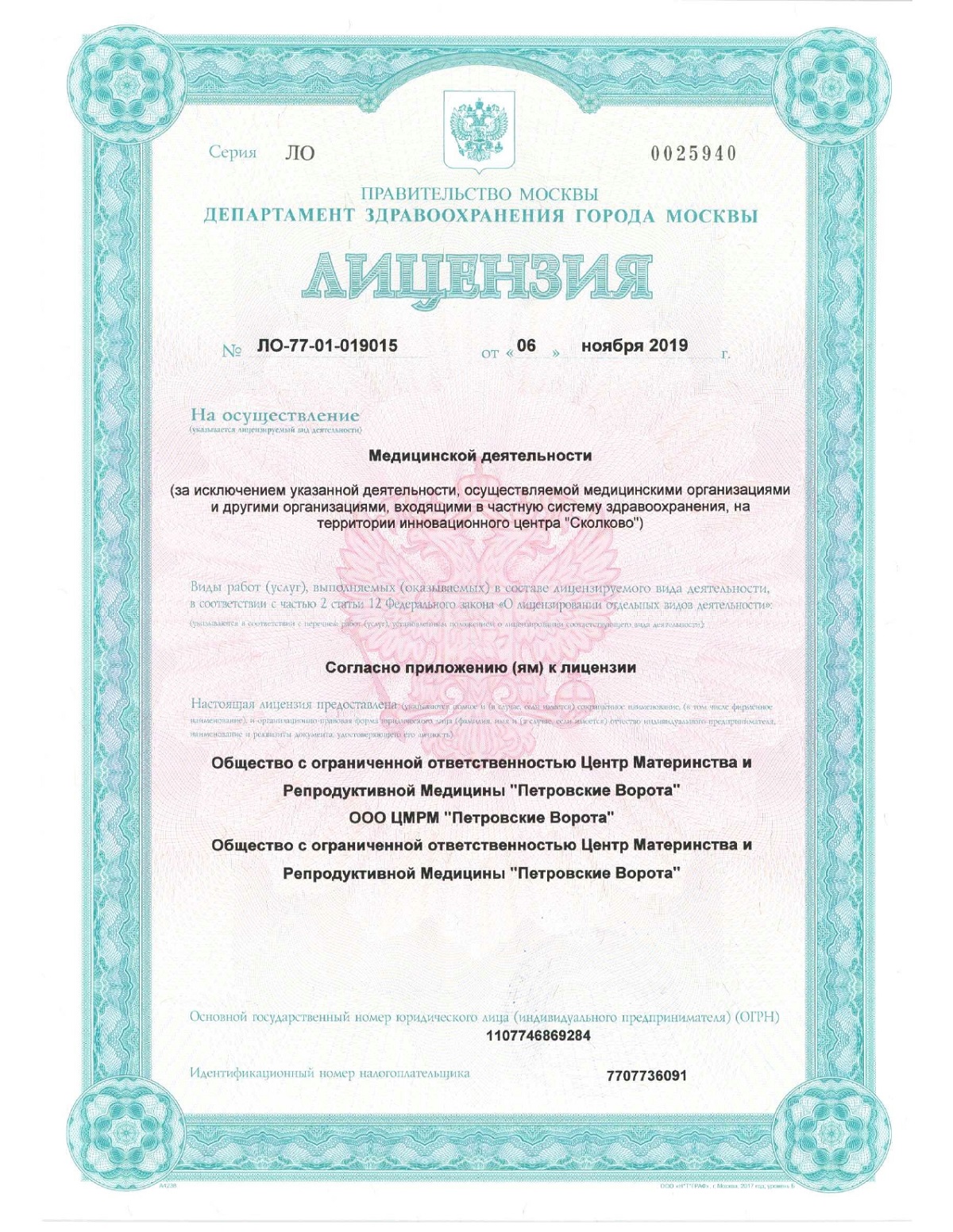
Surgery is the "gold standard" for radical treatment of a pilonidal cyst. Its goal is complete excision of the pathological tract, including all its branches and primary openings. Only this intervention guarantees a full recovery and eliminates the risk of recurrence. All surgeries at our Moscow clinic are performed by experienced surgeons using modern anesthesia techniques, ensuring patient comfort and safety.
Classical Methods
Classical surgeries include radical excision of the epithelial coccygeal tract. This technique involves removing a single block of skin and subcutaneous tissue containing the tract itself and all the affected tissue. After excision, the resulting wound can be sutured tightly, sutured to the bottom (marsupialization technique), or left open to heal.
Despite their high effectiveness, traditional surgeries have significant drawbacks:
- Trauma. A significant amount of healthy tissue is removed.
- Long recovery period. The healing period can last from several weeks to several months, requiring regular dressing changes.
- Severe pain in the postoperative period.
- Formation of a rough scar, which can cause discomfort.
That is why modern surgery increasingly favors minimally invasive techniques, which will be discussed below.
Minimally invasive methods.
The desire to minimize surgical trauma, shorten the recovery period, and improve cosmetic results has led to the development of minimally invasive techniques. Our Moscow clinic actively uses modern approaches that allow for the effective treatment of pilonidal cysts with minimal discomfort for the patient. Such surgeries are often performed as "same-day surgery." After a thorough diagnosis and brief preparation, the doctor selects the optimal method.
Such techniques include various plastic surgeries (e.g., the Karydakis procedure, Bascom procedure), in which excision of the epithelial coccygeal duct is combined with skin flap displacement. This allows the postoperative suture to be removed from the intergluteal fold, improving healing conditions and reducing the risk of recurrence. However, a real breakthrough in the treatment of epithelial coccygeal duct disease has been the use of laser technology.
Laser technology (SiLaC)
Laser treatment of the epithelial coccygeal duct (SiLaC — Sinus Laser-Assisted Closure) is the most modern and gentle surgical procedure. It is ideal for uncomplicated forms of the disease and achieves excellent results without large incisions.
The procedure involves the surgeon inserting a thin radial light guide into the affected canal through one of the primary openings. Laser energy is applied to the light guide, gently and controlled "burning" (coagulating) the epithelium lining the walls of the canal and all inflamed tissue. The affected canal collapses and "seals," turning into a connective tissue strand, and the laser itself is gradually removed.
Advantages of the laser method:
- Minimally invasive. No incisions; the surgery is performed through existing pinpoint openings. Healthy tissue is not affected.
- Fast recovery. The patient can return to normal activities in a short time. Sitting is permitted the next day.
- Excellent cosmetic results. No incisions mean no scarring.
- Low pain. Postoperative discomfort is minimal.
- Highly effective. When used correctly, this method provides a radical cure and a low risk of recurrence.
This intervention is the best help for patients who value their time and want the most comfortable treatment possible.
When to see a doctor
Don't delay your visit to the clinic or wait for a harmless symptom to develop into an acute abscess. Schedule a consultation with a surgeon if any of the following signs indicate inflammation:
- Pain or discomfort in the coccyx area
- Lump, swelling, or redness of the skin
- Any discharge from the intergluteal fold openings
The sooner diagnosis and treatment are initiated, the easier and faster it will be, and the higher the likelihood of using minimally invasive techniques.

Frequently Asked Questions
Is it possible to completely cure epithelial coccygeal tract without surgery?
No, conservative therapy is ineffective for complete recovery, as it doesn't address the underlying cause—the epithelium lining the canal. Only radical surgical intervention guarantees recovery.
How painful is the surgery?
Any surgery at our clinic is performed under effective anesthesia. After minimally invasive and laser procedures, pain is minimal and easily controlled with standard painkillers prescribed by your doctor.
How long does it take to recover from laser treatment?
The laser method is characterized by a very short recovery period. Patients typically return to office work and normal activities within 1-3 days after the procedure.
Will there be a scar after cyst removal?
Traditional excision leaves a linear scar. The advantage of laser treatment is that it is performed through pinpoint punctures, so there are no visible scars, ensuring an excellent cosmetic result.

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price



































































Definition and General Information
The epithelial coccygeal tract is a congenital narrow canal located under the skin in the intergluteal fold of the sacrococcygeal region, with one or more small openings on the skin's surface. It may not cause discomfort for decades, but under certain conditions, its active, inflammatory phase can become a serious medical problem.
Our Moscow clinic specializes in modern approaches to treating this condition. We understand that every symptom requires attention, and our primary goal is to provide qualified care. The only radical method that allows for the complete removal of pathological tissue and the resolution of the problem is surgical excision of the epithelial coccygeal tract.
Depending on the stage and form of the disease, either a classic excision of the epithelial coccygeal tract or a gentle laser procedure can be performed. Any treatment begins with an accurate diagnosis, and preparation for the procedure and the recovery period must be strictly monitored. If you're looking for effective treatment for ECC, don't delay your visit to the doctor – you can schedule a consultation today.