Anal Fissure Treatment
Anal fissures are a common proctological problem affecting both men and women. This condition causes emotional and physical discomfort due to the disruption of the anal mucosa.

specialists

equipment

treatment
Symptoms and causes of anal fissure
The main signs of an anal fissure are sharp pain in the anus immediately after urinating, especially when straining. The pain is so severe, it feels like a knife is being cut from the inside. Sometimes, itching or discomfort around the anus is felt. Bright red bleeding may be observed, visible on toilet paper or in the toilet bowl. Another symptom is a fear of urinating due to pain, which can lead to constipation. All of these symptoms together indicate damage to the mucous membrane around the anus.
Symptoms in the acute form
In an acute anal fissure, the symptoms are severe—a person experiences intense, literally piercing pain every time they urinate. Scarlet blood often appears on the surface of stool or toilet paper. An acute condition means the fissure is fresh, so the pain is intense.
Symptoms of the chronic form
With a chronic anal fissure, a person can suffer from its symptoms for months or years. Pain becomes a familiar companion to every visit to the toilet, although it is often milder than in acute cases. A feeling of heaviness or incomplete bowel movement may develop. Bleeding also occurs, but less frequently and less profusely.
Causes of anal fissure
The condition most often occurs due to trauma to the anus from hard or dry stool. When a person suffers from chronic constipation and is forced to strain intensely, the hard mass traumatizes the delicate mucous membrane, causing a deep tear.
Anal fissures can also be caused by infections and inflammations of the rectum, frequent diarrhea, fluid deficiency, and poor diet. The risk of fissures is increased by anatomical factors such as a narrow anus, poor diet, excessive physical exertion, and injury. People with a sedentary lifestyle are most susceptible to the condition. In women, anal fissures can occur after pregnancy and childbirth.
Why do anal fissures become chronic?
An acute anal fissure becomes chronic if the underlying cause isn't addressed promptly. Constant trauma interferes with healing. The body triggers a defense mechanism, creating fibrous tissue changes, creating a vicious cycle: inflammation intensifies muscle spasms, impairing circulation and slowing recovery.

Classification of anal fissures
To understand the specific features of the condition, doctors have developed a classification of anal fissures. Firstly, there are two main forms of the disease: acute and chronic. Secondly, the pathology is divided into different types based on localization—the location of the anal fissure.
Most often, it forms on the posterior wall of the anal canal, and slightly less commonly on the anterior wall. Finally, the third classification is based on the duration of the fissure. This distinguishes between newly formed defects and those that have existed for more than three months.

Pathogenesis of anal fissure
The pathogenesis of anal fissures is as follows: the condition begins with mechanical damage to the anal mucosa. For example, hard, dry stool scratches the sensitive surface, creating a deep wound. This damage triggers an inflammatory process, which increases the sensitivity of the nerve fibers.
This causes a sharp pain sensation and disruption of the blood supply to the damaged area. If the situation persists for a long time, the body adapts to constant inflammation, leading to serious complications.

Diagnosing Anal Fissure
A doctor can easily determine the presence of an anal fissure through palpation and visual examination. For a precise diagnosis, the doctor prescribes an anoscopy. The doctor carefully inserts an anoscope and examines the walls of the anal canal, identifies the fissure, assesses its extent, and determines any potential complications.
In addition, the doctor collects a medical history and asks the patient about the nature of pain, the presence of blood in the stool, and difficulty defecating. Palpation (feeling with a finger) and a rectal examination are used to confirm the diagnosis. It is important to rule out other conditions, such as hemorrhoids or polyps, to prescribe the correct treatment. Rectosigmoidoscopy, flora culture, and a complete blood count and stool test are also used for diagnostic purposes.
Anal Fissure Treatment
In the acute form, the patient is prescribed conservative treatment (topical and oral medications) aimed at reducing pain and healing the wound. The doctor will prescribe ointments, suppositories, and other medications that relax the anal muscles, improve blood flow, and accelerate healing. An enema can also help facilitate bowel movements. In the chronic form, accompanied by the appearance of tubercles, surgery is indicated.
If you have an anal fissure, you should follow a special diet. Eliminate salty and fatty foods, as well as alcohol. Fermented milk products and foods rich in fiber will help normalize bowel movements. To reduce stool trauma to the wound, you should maintain a hydration regimen and eat hot first courses daily. It is also recommended to regularly eat beets with sunflower oil, prunes, dried apricots, and porridge.
But if the fissure becomes chronic, conservative treatments are no longer effective. Then the question of surgical intervention arises. The aim of the surgery is to eliminate the cause of the spasm and improve blood circulation in the affected area.
After the procedure, it is important to follow the doctor's recommendations, maintain good hygiene, eat a healthy diet, and avoid physical activity. A comprehensive approach allows you to successfully manage the problem and prevent recurrence.
Conservative Treatment
Conservative treatment can help alleviate the symptoms of anal fissures and promote rapid wound healing. The patient is prescribed special ointments, suppositories, and baths that contain ingredients that help reduce inflammation, relieve pain, and accelerate tissue regeneration. A diet high in fiber-rich plant foods and adequate water intake are also recommended.
Surgical Treatment
When conservative treatments are ineffective, surgery is necessary. There are two main types of surgery: fissure excision and sphincterotomy.
Excision involves complete removal of the fissure itself, including the edges and scar tissue. The second option is sphincterotomy. Here, the doctor's goal is to reduce pressure on the anus by partially dissecting the internal sphincter.
Medications
Medications play an important role in the treatment of anal fissures. To alleviate the patient's condition, doctors prescribe the following groups of medications:
- Painkillers
- Anti-spasmodics
- Anti-inflammatory
- Healing
The doctor selects a specific medication, taking into account the individual characteristics of the patient and the severity of the condition. Self-selection of medications is not recommended, as this can worsen the situation.
Alternative Treatments
Traditional remedies for anal fissures include decoctions of chamomile, calendula, and oak bark—they reduce inflammation and accelerate healing. Warm baths with these infusions are also helpful. Various oils and poultices are also used. It's important to remember that any alternative treatments should be discussed with your doctor.

Complications of anal fissure
Delayed treatment can lead to heavy bleeding and the development of malignant and benign tumors. A wound that doesn't heal quickly can lead to the formation of a fistula, a tube connecting the rectum to the skin around the anus.
Another unpleasant consequence is infection, which can cause an abscess and severe pain. This is because during bowel movements, the bleeding wound regularly comes into contact with feces, which may contain dangerous bacteria. Pathogenic microorganisms settling on the fissure lead to infection and aggravate the inflammatory process.
In rare cases, malignant tissue degeneration may occur, requiring immediate medical intervention. The best prevention of anal fissures is an active lifestyle, a balanced diet, and avoiding constipation.
When to see a doctor
If you experience pain that intensifies during bowel movements, notice blood on the surface of your stool, on paper, or in the toilet bowl, or feel irritation or discomfort in the anal area, be sure to consult a proctologist. Even one of these symptoms may indicate an anal fissure.

The presence of anal fissures can be determined by the following symptoms:
- Pain in the anus both during and after bowel movements
- Blood discharge during bowel movements
- Spasm of the anus
- Itching of the anus
Prognosis and prevention
With prompt medical attention and proper treatment, most patients successfully recover from an anal fissure. The prognosis is generally favorable. However, there is a risk of recurrence. Prevention includes physical activity, proper nutrition, and good hygiene.

Frequently Asked Questions
Why does it hurt when going to the toilet?
Because this area is particularly sensitive—any touch or stretch causes severe pain.
How can you tell if it's a crack?
A characteristic symptom is a sudden, sharp pain when going to the toilet, followed by some relief, and then a return of the discomfort after some time. Traces of fresh blood may be seen on the toilet paper.
How long does it take for an anal fissure to heal?
1-2 weeks with proper treatment. However, if the disease has become chronic, the recovery period can increase to several months.
Why is an anal fissure dangerous?
The main dangers of an anal fissure are infection through the open wound, becoming chronic, and the formation of fistulas—channels between the internal opening and the skin that can lead to serious problems.
Can an anal fissure heal on its own?
Sometimes, eliminating the cause of the fissure, such as normalizing bowel movements, changing your diet, or eliminating straining during bowel movements, can help resolve the condition, but without specific treatment, the condition rarely resolves completely.

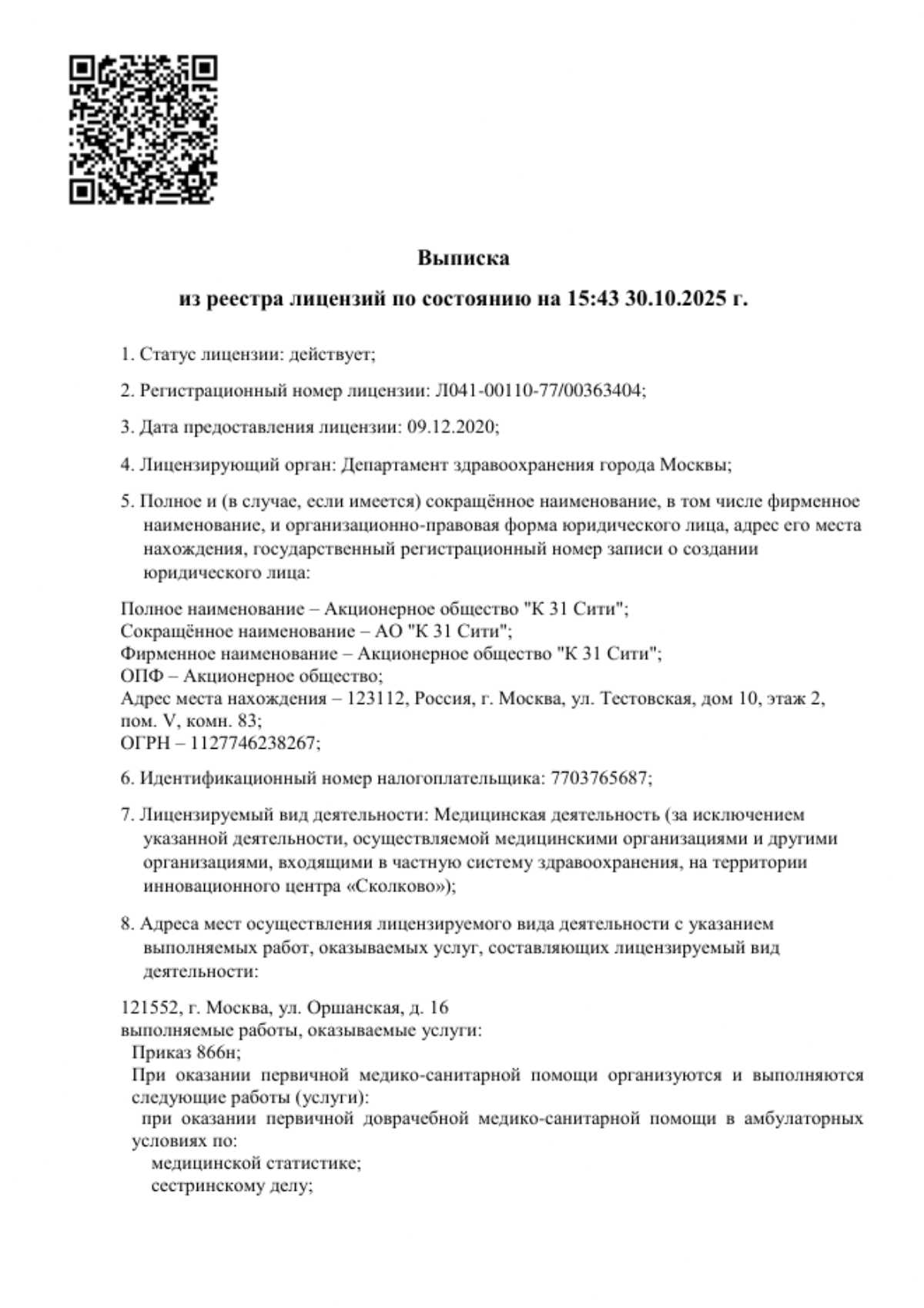
This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price
Other services



























Definition of anal fissure
An anal fissure is a small tear inside the anus, specifically in the inner lining of the anal canal. It occurs where stool passes during bowel movements. This damage makes defecation painful, sometimes even causing bleeding.
This defect is also called a rectal fissure because it is located in the anal area. Treatment for an anal fissure includes the use of ointments, suppositories, special baths, and dietary changes to soften the stool and reduce pain.