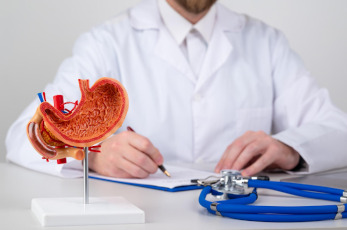
Gastric resection – stomach reduction surgery for weight loss
When conservative therapy – diets, exercise, medications – has exhausted itself, and the numbers on the scale continue to threaten health, bariatric surgery comes to the forefront. And its most effective tool in the fight against morbid obesity is gastric resection.
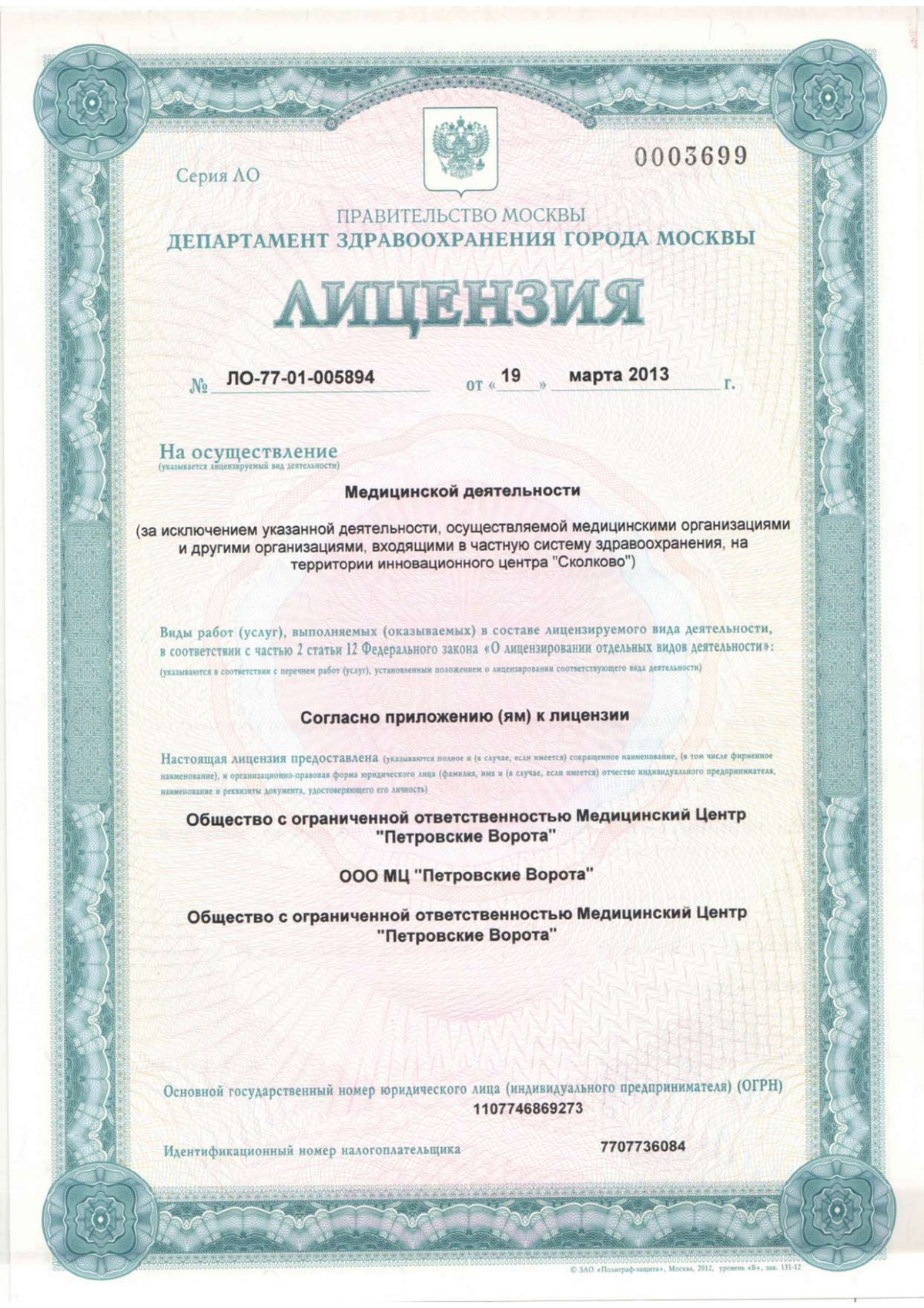
Let's be clear: this has nothing to do with cosmetology. This is not a whim, but a serious surgical treatment. Its goal is to achieve dramatic and, more importantly, sustainable weight loss through irreversible stomach reduction. At the Bariatric Center of the K+31 Clinic (Moscow), we approach this surgery as a fundamental step in the treatment of metabolic syndrome. For us, every patient is a unique clinical challenge, requiring a meticulous approach, starting from the very first consultation.

specialists

equipment

treatment
History of gastric resection
The idea of resection itself is not new. Its history dates back to the 19th century, to the work of Theodor Billroth, who performed this operation in 1881 to save a patient from cancer. For decades, it has been used in oncology and the treatment of peptic ulcers. Adapting this technique for bariatrics is medicine's response to the obesity epidemic that began in the second half of the 20th century.
Naturally, technology has changed dramatically. Open, traumatic interventions have given way to laparoscopic surgery. Today, this is the "gold standard" that our bariatric center in Moscow uses for the vast majority of patients.

Indications for gastric resection
A surgeon performs a gastric resection not at the patient's request, but for strict medical reasons. This is not a way to "lose weight quickly for the summer." The primary indication is severe, morbid obesity that is unresponsive to any other treatment methods. The selection criterion is objective—Body Mass Index (BMI).
Who needs surgery?
So, when does surgery become necessary?
- A BMI of 40 kg/m² or higher is an absolute indication. Stage III obesity is a serious condition in its own right, requiring radical measures.
- A BMI of 35-39.9 kg/m², however, brings with it a whole host of problems: type 2 diabetes, uncontrolled hypertension, severe sleep apnea (stopping breathing), and painful joints requiring replacement. In such cases, weight loss is the main factor in treating the underlying condition.
The key is the patient's willingness to change. Surgery is just a tool. A powerful and effective one, but still a tool. Success 90% depends on how the patient uses it for the rest of their life. Therefore, the final decision is made only after working with the patient and carefully assessing all the pros and cons.

Contraindications to gastric resection
Of course, gastric resection surgery is not a panacea available to everyone. There is a clear list of contraindications that we, as doctors, are obliged to exclude. Patient safety is an absolute, non-negotiable priority here. We divide contraindications into two groups: absolute, when surgery is fundamentally impossible, and relative, which require either preliminary correction or a particularly balanced approach.
Absolute contraindications, or when we say "no":
- Severe, decompensated heart and lung diseases. Simply put, if the anesthetic risk outweighs the potential benefit of the surgery.
- Active infectious processes.
- Pregnancy. This is an axiom; any planned surgical intervention during this period is excluded.
- Age under 18
- Severe, uncontrolled mental disorders, as well as alcohol or drug addiction. The patient must be able to adequately follow all postoperative recommendations, otherwise, treatment is pointless.
- Active cancer (not related to the stomach)
Relative contraindications - situations requiring attention:
- Exacerbation of chronic gastrointestinal diseases, such as peptic ulcer disease. It is necessary to first achieve stable remission.
- Certain endocrine disorders that must be corrected before surgery.
- The patient's psychological unpreparedness. If the doctor sees that the patient does not understand the full complexity and responsibility, the surgery will be postponed.
Types of gastric resection
Longitudinal resection
Sleeve gastrectomy, also known as sleeve gastrectomy, is the "workhorse" of modern bariatric surgery. It involves removing the larger, more distensible portion of the stomach, namely the greater curvature and fundus.
A narrow tube, a "sleeve," is formed from the remaining lesser curvature, holding no more than 100-150 ml of volume. This type of resection has two effects, as we've already discussed: mechanical restriction and hormonal changes. A key advantage is that it maintains the normal flow of food through the gastrointestinal tract. The intestines are not excluded from digestion, minimizing future problems with vitamin and mineral absorption.
Laparoscopic resection
It's important to understand: laparoscopic resection is not a separate type of surgery, but a surgical approach. It's how we operate. Today, most bariatric procedures at our Moscow center are performed laparoscopically.
Instead of one large incision, several 5-15 mm punctures are made. A camera and ultra-fine instruments are inserted through these punctures. The surgeon sees the surgical site on a monitor in HD with multiple magnification, allowing for pinpoint precision. The benefits for the patient are clear: minimal pain, rapid recovery, and virtually no scarring.
Resection for oncological diseases
Here, the goals and objectives are completely different. This is not bariatric surgery. The focus is not on weight loss, but on radical tumor removal, adhering to all oncological principles. The extent of resection can be distal, proximal, and sometimes complete organ removal—a total gastrectomy—is required. These are technically much more complex procedures, which always include lymph node dissection (removal of the lymph nodes).
Preparing for surgery
Preparing for gastric resection surgery is, without exaggeration, half the battle. It's not a routine blood test the day before hospitalization. At our clinic, it's a multi-stage process that begins weeks, and sometimes months, before the procedure itself. Our goal is to approach the surgery with a patient who is fully examined, has received the best possible treatment for all comorbidities, and, equally important, is psychologically prepared.
The preparation process is built on several fundamental principles.
1. Тотальное медицинское обследование
Мы должны знать о пациенте все. Врач назначает спектр исследований, чтобы получить полную картину состояния здоровья. Это карта, по которой мы прокладываем безопасный маршрут.
- Лабораторный комплекс. В него входит все: от общего анализа крови и коагулограммы (основной показатель свертываемости) до биохимии с печеночными и почечными показателями, липидного профиля, уровня гормонов щитовидной железы, гликированного гемоглобина, а также статуса по основным витаминам и микроэлементам. Обязательны анализы на госпитальные инфекции
- Инструментальная диагностика. ЭКГ – стандарт. УЗИ органов брюшной полости — обязательно, мы должны оценить состояние печени, желчного пузыря, поджелудочной. Рентген легких или КТ. Спирометрия – важное исследование для оценки функции внешнего дыхания у пациентов с тяжелым ожирением
- Эзофагогастродуоденоскопия (ЭГДС). Это «золотой стандарт». Мы должны заглянуть внутрь и убедиться, что слизистая пищевода, желудка и двенадцатиперстной кишки готова к операции. Никаких активных язв, эрозий или выраженного воспаления быть не должно. Если они есть — сначала проводим лечение
- Консультации смежных специалистов. Пациента в обязательном порядке смотрят терапевт, кардиолог, эндокринолог. И, конечно, анестезиолог — именно он дает финальное заключение о переносимости наркоза
2. Предоперационная диета
За 2-4 недели до операции мы назначаем специальную диету с низким содержанием углеводов и жиров. Зачем? Главная цель — уменьшать размеры печени. У пациентов с морбидным ожирением печень часто увеличена из-за жирового гепатоза. Уменьшенная, «сдувшаяся» печень значительно облегчает хирургический доступ к верхней части желудка во время лапароскопической операции, делая ее технически проще и безопаснее.
3. Психологическая готовность
Резекция желудка — это инструмент, а не волшебная палочка. Успех напрямую зависит от пожизненного соблюдения правил питания. Консультация с клиническим психологом помогает пациенту выстроить реалистичные ожидания и осознать всю меру ответственности.
4. Финальный этап подготовки
Накануне операции – легкая жидкая пища. С вечера и утром в день вмешательства – полный голод, нельзя ни есть, ни пить. Это стандартный протокол для обеспечения безопасности во время наркоза.
Treatment, rehabilitation, prevention
Диета после резекции желудка
Процесс не ограничивается поверхностным воспалением. Инфекция быстро распространяется вглубь, разрушая окружающие структуры. Питание после операции — это базис, на котором строится весь дальнейший успех. И это новый образ жизни. Пациент должен понимать: теперь его желудок имеет принципиально другой объем и функционирует иначе.
Главные принципы, которые становятся законом:
-
Поэтапность. Переход от жидкости к твердой пище происходит постепенно, в течение 4-6 недель. Сначала вода и бульоны, затем пюре, и только потом — мелко измельченная твердая пища.
-
Объем порции. Он минимален. Начинаем с 30-50 мл и постепенно доходим до 150-200 мл. Это максимальный объем на один прием пищи.
-
Приоритет белка. Основа рациона — белок (мясо, птица, рыба, творог, яйца). Это строительный материал для организма, который предотвращает потерю мышечной массы на фоне активного похудения.
-
Тщательное пережевывание. Каждый кусок должен быть пережеван до состояния кашицы.
-
Разделение еды и питья. Жидкость пьется либо за 30 минут до еды, либо через 30-60 минут после. Пить во время еды нельзя — вода вытолкнет пищу из малого желудка, и чувство сытости не наступит.
Цены на резекцию желудка
Вопрос стоимости всегда важен. Итоговая цена на лечение зависит от множества факторов: вида и сложности самой операции (продольная, дистальная, проксимальная), использования конкретных расходных материалов, длительности госпитализации. Ниже представлен ориентировочный прайс на основные виды вмешательств в нашем центре в Москве. Точная стоимость всегда рассчитывается индивидуально после консультации хирурга.
- Резекция желудка парциальная — от 137 200 руб.
- Резекция желудка — от 186 200 руб.
- Резекция желудка лапароскопическая — от 254 700 руб.
- Продольная резекция желудка лапароскопическая (Sleeve) — от 222 900 руб.
- Резекция желудка проксимальная субтотальная трансторакальная — от 462 000 рубл.

Литература и источники
Данный материал подготовлен на основе анализа актуальных клинических рекомендаций и фундаментальных работ в области бариатрической и метаболической хирургии.
- Национальные клинические рекомендации по лечению морбидного ожирения у взрослых / Российское общество хирургов, Общество бариатрических хирургов. — М., 2022.
- Яшков Ю.И. Хирургия метаболического синдрома. — М.: Медпрактика-М, 2017. — 260 с.
- «Бариатрическая хирургия» — учебно-методическое пособие под редакцией В. А. Кащенко и соавторов, Санкт-Петербург, 2020
- Обзор современных представлений о бариатрической хирургии: современные методы и техника / Доказательная гастроэнтерология. — 2023. — №3.
- Обзор осложнений бариатрической хирургии и их профилактика / Ростовский государственный медицинский университет. — 2024.

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price





































































What is gastric resection?
What actually happens during the surgery? Simply put, gastrectomy is the surgical removal of most of the stomach (approximately 80%). The surgeon literally performs anatomical cutting of the organ, forming it into a narrow tube. As a result of this procedure, the stomach's volume is reduced to 100-150 ml.
The practical consequence? Satiety occurs with a minimal amount of food. This is the restrictive component, that is, a purely mechanical limitation. Reducing calories becomes not an effort of will, but a physiological necessity.
But there is a second, no less important mechanism. During the resection, the fundus of the stomach is removed—the main site of ghrelin synthesis. This is the "hunger hormone." Without this site, there is no constant, painful desire to eat. The patient not only feels full faster, but also wants to eat less in general. This type of intervention, known internationally as sleeve gastrectomy, comprehensively changes the entire eating system.