Treatment of rectal prolapse
Rectal prolapse is a common disease in proctology and can occur in both adults and children. If symptoms appear, you should consult a proctologist for diagnosis. Timely detection of the disease allows you to get by with simpler methods of treatment, without the use of surgical intervention.
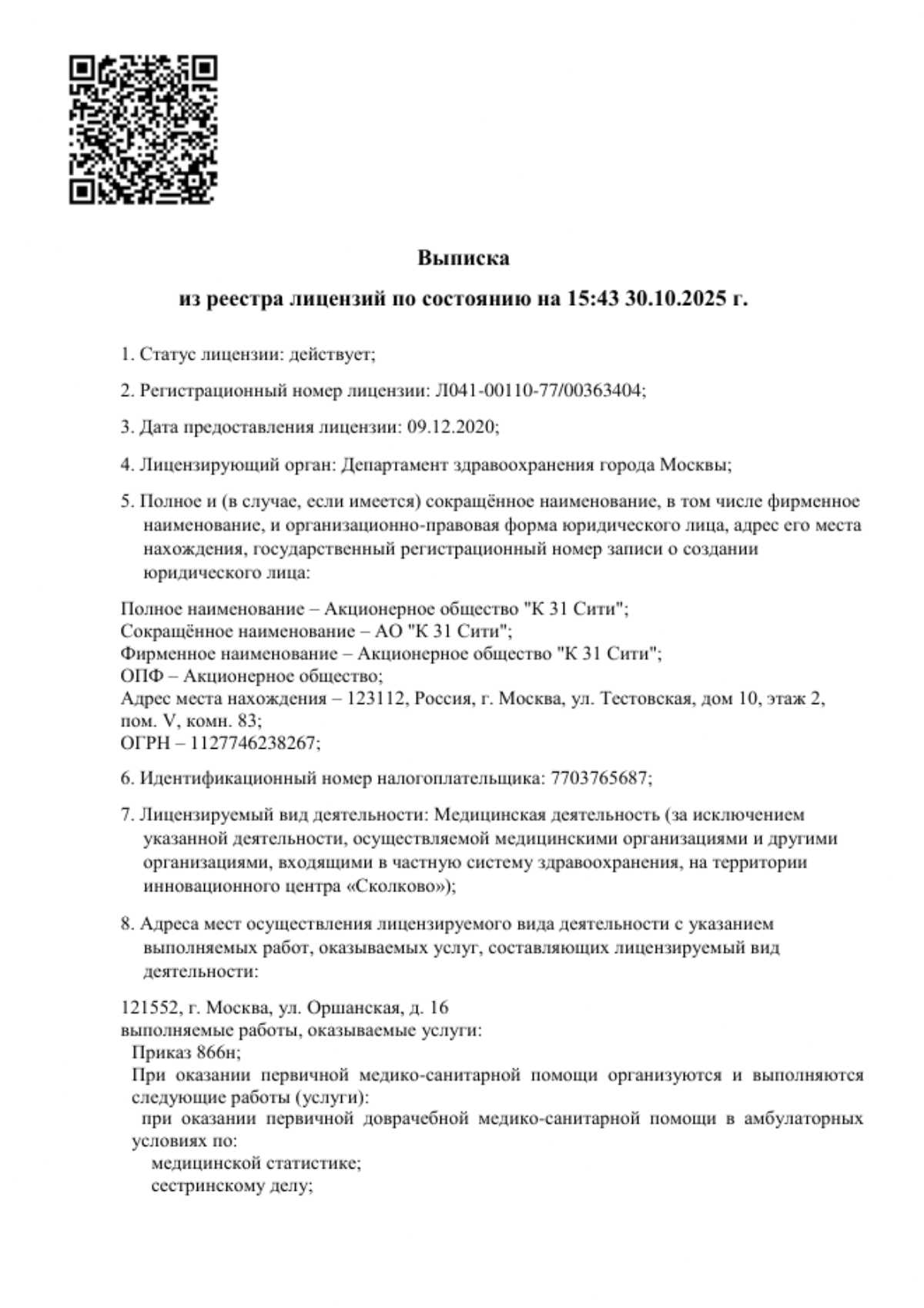
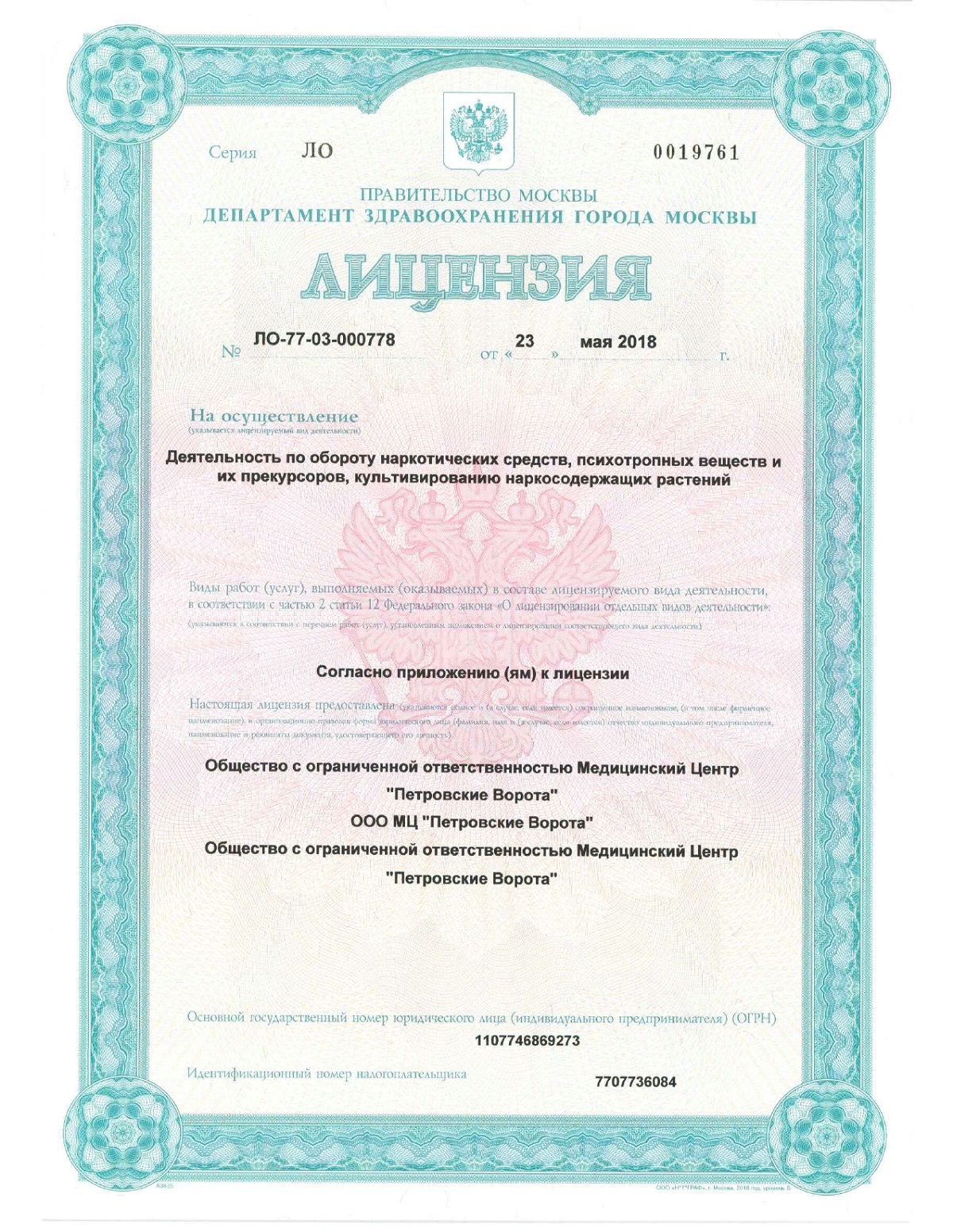
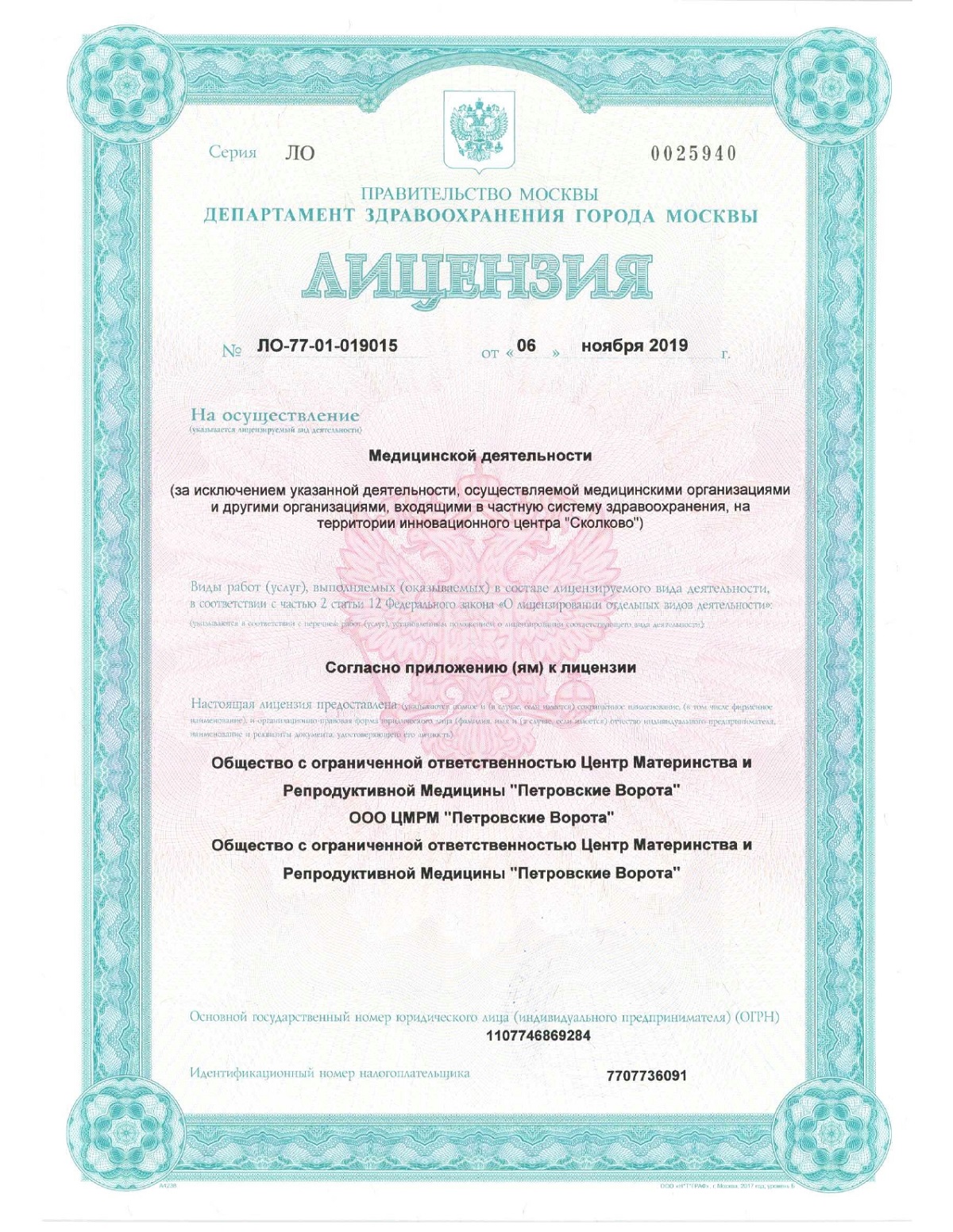
The K+31 clinic conducts examination and treatment of rectal diseases of varying complexity using modern conservative and radical methods.

specialists

equipment

treatment
General information about the disease
Prolapse of the rectum is more common in men. This is explained by different anatomical features of the internal structure of the pelvis (bones, shape and length of the sigmoid colon), as well as the fact that men experience greater physical exertion. Due to the specifics of the child's body, under the influence of various internal and external factors, the disease can also occur in young children (up to 4 years). The length of the prolapsed segment of the intestine can range from a few centimeters to 2/3 of its total length. The pathology develops over the years, causing pain and disrupting the process of defecation. The intestine can prolapse at one time or gradually, under the influence of constant loads.
Definition and main symptoms
Classification and stages
There are external and internal prolapses. In the case of external prolapse, the distal section passes through the rectal sphincter out of the anus. This can be observed both visually and by external palpation.
During internal prolapse (intussusception), the walls of the rectum are weakened and other parts of the intestine protrude into it, like a hernia. In this case, defecation is also disrupted and pain occurs, but it is impossible to palpate the prolapse from the anus, so the pathology is difficult to detect without a detailed examination.
There are various types of classifications of the disease. Depending on the nature of the occurrence, the following stages of intestinal prolapse are distinguished:
- Only during a visit to the toilet or straining
- When lifting weights and other physical activities
- Without strain, while walking
Depending on the degree of dysfunction of the muscular apparatus, the following stages are distinguished:
- Compensation - reduction occurs independently, under the action of the intestinal muscles
- Decompensation (late stage) - reduction is performed manually
A distinction is made between high and low severity intussusception with the formation of enterocele and sigmocele. In these cases, segments of the small intestine or sigmoid colon, respectively, exit through its wall into the rectal cavity.
The disease also has stages that depend on the insufficiency of the rectal sphincter (based on symptoms):
- It is difficult for a person to hold back gases, gas emission occurs uncontrollably
- The patient cannot hold back liquid stool, leakage occurs
- Spontaneous release of solid feces
With sphincter insufficiency of the 3rd degree, the patient cannot control the act of defecation. The condition appears with prolonged prolapse in an advanced stage.
Causes of rectal prolapse
Pathology can occur due to genetic predisposition or such anomalies as impaired intestinal wall formation, elongated sigmoid colon, which is laid down at birth and is more often diagnosed in children.
In adults, the following factors influence the development of the disease:
- Feature of the anatomical structure of the sacrum. Normally, the coccyx bone at the end of the spine has a rounded inward shape. This provides support for the internal organs of the pelvis and intestines. In case of congenital pathology or injury, the sacrum can be straight, which affects the loss of the supporting function
- Professional activities associated with lifting weights or physical activity (loaders, athletes).
- Pregnancy (especially multiple), as well as childbirth with complications
- Diseases that have affected the violation of the muscular layer of the rectum (intestinal tumors, urolithiasis, prostate adenoma, gastrointestinal pathologies with frequent diarrhea or constipation)
- Relaxation of the anal sphincter in people who engage in anal sex
In women with weakened pelvic floor muscles, rectal prolapse is often diagnosed simultaneously with prolapse/prolapse of the uterus, which can also be accompanied by urinary and fecal incontinence.
The factors that provoke the appearance of rectal prolapse include high intra-abdominal pressure as a result of prolonged coughing, frequent constipation, difficult childbirth, and sudden weight loss.
Etiology and pathogenesis
The pathology occurs due to weakness of the pelvic floor muscles under the influence of external factors that provoke an increase in pressure in the abdominal cavity. Scientists consider three factors that explain the mechanism of disease development:
- Hernial. According to this theory, due to tension and increased intra-abdominal pressure, segments of the small intestine accumulate in the Douglas pouch and begin to press on the rectum. As a result of pressure, the intestine begins to slide down, until it falls out of the anus.
- Invagination. It explains the occurrence of internal prolapse by the fact that first there is a weakening of the muscular-ligamentous apparatus, and then side effects occur, for example, cicatricial degeneration of the intestinal wall and protrusion of neighboring organs into the rectum.
- Neurogenic. The theory suggests that the cause of the development of pathology is a violation of the genital nerve with further prolapse of the internal organs and prolapse of the intestine from the anus
Clinical practice shows that most often the explanation of the mechanism of the disease is a combination of two theories at once and hernia is almost always present.
Symptoms, course, diagnostics
Treatment methods
Conservative treatment
It involves prescribing medications to relieve inflammation and normalize stool. The doctor prescribes a diet for the treatment and prevention of constipation, and, if necessary, selects laxatives.
Methods that are used in the early stages of the disease:
- Biofeedback therapy with gradual restoration of pelvic floor muscle tone
- Tibial neuromodulation with stimulation of the anal sphincter nerve
Methods of electrical stimulation to increase muscle activity are performed using special equipment. A good effect from the therapy will be in young patients at the first stage of prolapse. If bowel prolapse has been present for more than 3 years, the doctor selects a radical method of therapy.
Хирургическое лечение
Применяется на запущенных 2 и 3 стадии ректального пролапса. Существует несколько десятков техник хирургического вмешательства на прямой кишке. Хирург подбирает метод операции, в зависимости от тяжести заболевания, его типа и наличия осложнений.
При ущемлении выпавшей кишки операцию проводят в экстренном порядке. В других случаях назначается плановое хирургическое вмешательство открытым или лапароскопическим методом, как через промежность, так и через разрез брюшной стенки.
Операция включает три этапа:
- Резекция выпавшего отдела кишки. Врач отсекает лишние ткани дистального отдела прямой кишки, выходящие за пределы анального кольца. Используется несколько техник — циркулярное, лоскутное сечение, резекция и наложение шва на мышечную стенку и др.
- Фиксация кишки внутри. Врач подшивает оставшуюся прямую кишку к продольным связкам позвоночника или крестца
- Пластика анального сфинктера. Выполняется сужение отверстия и коррекция мягких тканей с использованием специальных материалов. Мышцы леваторы подшивают к прямой кишке
Современные лапароскопические операции позволяют избежать больших внешних разрезов и ускорить время на реабилитацию после вмешательства. Все внутренние манипуляции хирург проводит с помощью лапароскопического оборудования, которое устанавливается через трубки в брюшную стенку или в заднепаховую область. Это малотравматичный метод, после которого восстановление организма проходит быстрее.
При наличии осложнений и некроза участка прямой кишки сначала выполняется резекция, а затем наложение сигмостомы на поврежденный участок. При этом хирургическое вмешательство проходит только открытым способом.
Rehabilitation
In the first week after the operation, the patient takes medications to relieve swelling and pain, and prevent infections. It is also necessary to treat the postoperative wound with an antiseptic and change sterile dressings. In the postoperative period, it is important to exclude any straining, so it is necessary to avoid constipation, coughing, and lifting heavy objects (more than 5 kg).
After discharge from the hospital, for 21 days after the operation, a diet is recommended to normalize the gastrointestinal tract and stool consistency. It is recommended to consume fiber and plenty of water. The patient can move independently, but it is important to exclude any physical activity.
A month after the operation, you can begin to do exercises to strengthen the pelvic floor muscles. Kegel exercises, biofeedback therapy, and physiotherapy are suitable for this. All procedures are carried out in courses, under the supervision of a doctor.
Prevention and recommendations
To prevent recurrent rectal prolapse, doctors recommend eliminating risk factors. Gastrointestinal and pulmonary diseases should be treated promptly to prevent prolonged coughing, constipation, and prolonged diarrhea. It is also necessary to control physical activity and prevent complications after childbirth.
To prevent complications in cases of prolapse that have already occurred, it is necessary to undergo an examination by a proctologist and conservative therapy.
When to see a doctor
If you experience pain in the anus, accompanied by bleeding, protrusion of a part of the rectum that is difficult to put back in, you should see a proctologist.
If the rectum is strangulated, there is severe, sharp pain that intensifies when you try to put it back in on your own. In this case, you need a doctor's help.
To make an appointment with a proctologist at any department of the K+31 clinic in Moscow, you can call the reception or use the WhatsApp chat.

Questions and Answers
What is the difference between hemorrhoids and rectal prolapse?
With hemorrhoids, the sphincter is very tense, hemorrhoidal nodes protrude from one or more sides. With rectal prolapse, it is the intestine without nodes that protrudes, and the sphincter is relaxed.
How to cure rectal prolapse without surgery?
Rectal prolapse can be treated without surgery only in the early stages. In this case, neurostimulation of the pelvic floor muscles and sphincter is performed using special equipment.
What should not be done after rectal surgery?
After rectal surgery, it is important to avoid constipation, heavy lifting, and anal sex. This will help avoid relapse, pain, and re-injury.
Sources and literature
- Vorobyov G.I., Shelygin Yu.A., Orlova L.P., Titov A.Yu., Kapuller L.L., Podmarenkova L.F., Zarodnyuk I.V., Kabanova I.N., Langner A.V. Clinic, diagnostics and treatment of patients with rectal prolapse. Russian Journal of Gastroenterology, Hepatology, Proctology. 1996. Vol.6: 78-82
- Modern concept of surgical treatment of rectal prolapse / Musin A.I., Blagodarny L.A., Frolov S.A. // Astrakhan Medical Journal - 2011
- Shelygin Yu.A. Clinical guidelines. Rectal prolapse / Association of Proctologists of Russia: 2021 https://akr-online.ru/upload/iblock/44f/%D0%9A%D0%A0177%20%D0%92%D1%8B%D0%BF%D0%B0%D0%B4%D0%B5% D0%BD%D0%B8%D0%B5%20%D0%BF%D1%80%D1%8F%D0%BC%D0%BE%D0%B9%20%D0%BA%D0%B8%D1%88%D0%BA%D0%B8%20K62.3.pdf

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price


































































What is rectal prolapse?
Prolapse is a partial or complete displacement of the rectum and its exit from the anus. In this case, the distal section, which is located closest to the sphincter, can protrude outward by 2-16 cm. Unlike hemorrhoids, with rectal prolapse, the intestine itself, not the hemorrhoidal nodes, protrudes beyond the anatomical boundaries, and the sphincter is relaxed.
At an early stage, the pathology periodically appears and disappears during straining, and as it progresses, it requires manual reduction. If the problem is left unattended, a gradual increase in the volume of the prolapsed intestine occurs with the risk of dangerous complications.