Lump on the Labia - Diagnosis and Treatment
A lump in the genital area that causes discomfort and rapidly changes in appearance is an alarming sign that requires the attention of a specialist. Such swelling can signal a variety of conditions, from mild to serious, including cancer.

specialists

equipment

treatment
Causes of the appearance of bumps and growths
The factors that trigger the development of neoplasms are varied and poorly understood. Chronic perineal trauma, hormonal imbalances, genital infections, the high-risk human papillomavirus (HPV), and inflammatory changes in the vaginal mucosa and labia all increase the risk of developing lumps.
Bartholin's gland cyst
A cyst is a fluid-filled sac that develops in a gland located at the entrance to the vagina. This gland typically produces a secretion that moisturizes the mucous membrane, helping to maintain comfort and hygiene.
Sometimes the gland's ducts become blocked, and fluid accumulates inside, forming a cyst. These growths vary in size, from very small to large, visible externally. They are usually painless and are discovered accidentally during a doctor's examination or self-examination.
Very often, a Bartholin gland cyst causes no discomfort and is discovered incidentally. If the lump is small, your doctor may recommend monitoring it without treatment. Some cysts may resolve on their own, but in some cases, the contents of the cyst become infected, causing inflammation and pain.
The infection is usually caused by bacteria entering the cyst. The woman then notices unpleasant symptoms: swelling, pain, and fever. This condition is called a Bartholin's gland abscess and requires immediate medical attention.
Condylomas
They are benign growths that resemble miniature papillary structures. Sometimes a single condyloma appears, but more often, entire clusters of growths, visually resembling a broccoli inflorescence, form.
Condylomas are caused by infection with the human papillomavirus, which is highly contagious and is transmitted primarily through close contact, including sexual intercourse and everyday situations, especially with poor personal hygiene.
Wart growth is triggered by a weakened immune system. The risk of developing a malignant form exists, although it is extremely low. Once the immune system is restored, the body is able to suppress viral activity on its own, leading to the disappearance of the condylomas. According to statistics, approximately eighty percent of such growths disappear spontaneously within a year or two after their appearance.
However, if the immune system remains weak, condylomas continue to develop, sometimes leading to precancerous skin changes that can develop into cancer.
Melanoma
This formation is a dangerous tumor arising from pigment cells called melanocytes. In the genital area, melanoma is localized primarily in the tissues of the labia majora and minora, as well as the clitoris. Elderly women who have passed menopause are most susceptible to the disease.
Outwardly, melanoma appears as a black or brown spot protruding from the skin. Multiple small satellite nodules often develop around the primary lesion. However, approximately one-third of cases are characterized by a lack of color, which complicates diagnosis.
Symptoms of the disease are varied and include a burning sensation, discomfort, pain, enlarged regional lymph nodes in the groin area, and the appearance of an unpleasant odor. The initial stage is asymptomatic, which explains the late detection of the pathology and a worse prognosis. Typical signs of melanoma development include erosion and bleeding from the surface of the lesion.
Vulvar cancer
Among the oncopathologies of the female external genitalia, epithelial cancers are common. These include, for example, Paget's disease, squamous cell carcinoma, basal cell carcinoma, and Merkel cell carcinoma. Squamous cell carcinoma is considered the most common type, accounting for 90% of cases. This is explained by the fact that the surface of the vulva is covered with squamous epithelial cells.
The main cause of cancer is considered to be hormonal imbalances before menopause. Changes in receptor sensitivity to the female hormone estrogen provoke structural changes in the mucous membranes. Cancerous diseases are often preceded by a number of chronic mucosal pathologies, such as leukoplakia, kraurosis, and atrophic dermatitis. One of the most significant precursor conditions is dysplasia.

Symptoms of Lumps and Growths
Small tumors in the female external genitalia usually go undetected. The only sign is the presence of the tumor, detected visually or by palpation. If the tumor grows, characteristic complaints may appear:
- Pain when moving, sitting, playing sports, or having sex
- Unusual vaginal discharge: blood, pus, or an unusual odor
- Feeling of a foreign object in the genital area
- Irregular menstrual cycles
- Problems with urination
- Swollen lymph nodes in the groin
- Constant fatigue, weakness
- Fever
The appearance of these warning signs signals the need for an urgent visit to the gynecologist. Early diagnosis significantly facilitates treatment and reduces the likelihood of adverse effects.

Diagnostics
Pathologies of the external genitalia are easily diagnosed by a simple visual examination and palpation by a specialist. To assess the depth and extent of the tumor, doctors also refer women for a range of diagnostic procedures:
- Examination with a special magnifying instrument (vulvoscopy)
- Examination of the cervix and vaginal walls (colposcopy)
- Endoscopic examination of the uterine cavity (hysteroscopy)
- Ultrasound scanning of the internal reproductive organs (transvaginal ultrasound)
- Computerized tomography or magnetic resonance imaging of the pelvic region
- Endoscopic examination of the inner surface of the intestine and bladder
To exclude possible concomitant sexually transmitted infections, PCR tests of blood and vaginal contents, and bacteriological culture of a vaginal smear are performed. A biopsy is also mandatory—a tissue sample from the tumor itself or a scraping from the edge of the resulting ulcers is taken to examine the tissue structure in detail and determine the tumor's nature.
The importance of differential diagnosis of hydrogenitic tumour (hidradenoma) is also worth noting. This helps distinguish this pathology from syphilis, as the symptoms of these two diseases can be similar.
Treatment of bumps and growths
A lump on the labia requires a careful approach to treatment. Doctors typically choose one of two main approaches: conservative or surgical. Conservative treatment is appropriate if the problem is minor. This approach is effective when the cause is clear and there is no health risk.
Surgery is recommended if the situation is serious: the lump is large, painful, interferes with normal functioning, or there is a risk of complications. Surgery allows for a complete solution to the problem and prevents potential complications.
Conservative treatment
If a lump on the labia is caused by a harmless condition, such as abnormal hair growth, surgery is not necessary. Special medications are sufficient, such as:
- Anti-inflammatory medications. These are cream-based formulations containing substances that reduce inflammation and prevent additional infection.
- Antibiotics. These are prescribed if the cause is a bacterial infection, such as in the case of inflammation of the labia or an abscess. These medications are selected individually after testing the microflora.
- Antiviral medications. These are used in the presence of herpes.
Sometimes these medications are ineffective, in which case the doctor may recommend surgery.
Surgical treatment
Invasive intervention is indicated in situations such as:
- Abscesses. When pus accumulates at the site of inflammation, whether it's a glandular cyst or a common pimple or boil, the doctor makes a skin incision, cleans the cavity of pus, and inserts a special tube to drain the fluid.
- Cysts and atheromas. This surgery aims to remove fluid-filled capsules or inflammatory lesions in the sebaceous glands.
- Condylomas and papillomas. Benign lumps in the genital area are treated with modern methods: laser, radio waves, or cold (called cryodestruction).
Most problems are resolved with mini-surgeries under local anesthesia. The procedure is quick and gentle, and the patient returns home soon after. Sometimes there's a choice between surgical and conservative treatment, as in the case of a hemangioma. The decision is always made solely by the doctor.
Complications and Prognosis
Growths on the labia are most often harmless and easily treated, especially if a woman seeks medical attention promptly. However, delaying a visit to a specialist can have serious consequences. Even benign growths can increase in size, becoming inflammatory. Some cases are accompanied by the accumulation of pus and the development of abscesses. Polypous structures tend to degenerate into tumors.
Malignant lesions of the female external reproductive organs pose a serious threat to health and life. If pathological tumor growth is not diagnosed promptly, secondary lesions develop in vital structures and the lymphatic system, causing severe poisoning of the body, which often leads to the patient's death.

When to see a doctor
A lump in the genital area is a compelling reason to consult a specialist, regardless of discomfort. You should see a doctor immediately if you experience pain (especially if it increases), tissue redness, difficulty moving, pus, or other discharge.
Prices for treating a lump on the labia in Moscow
The cost of treating a growth on the labia in Moscow depends on several factors. First, the diagnosis is important—a simple inflammation is one thing, while a serious illness is quite another. The procedures and medications required depend on the diagnosis. Another important factor in pricing is the clinic's level and the doctors' qualifications.
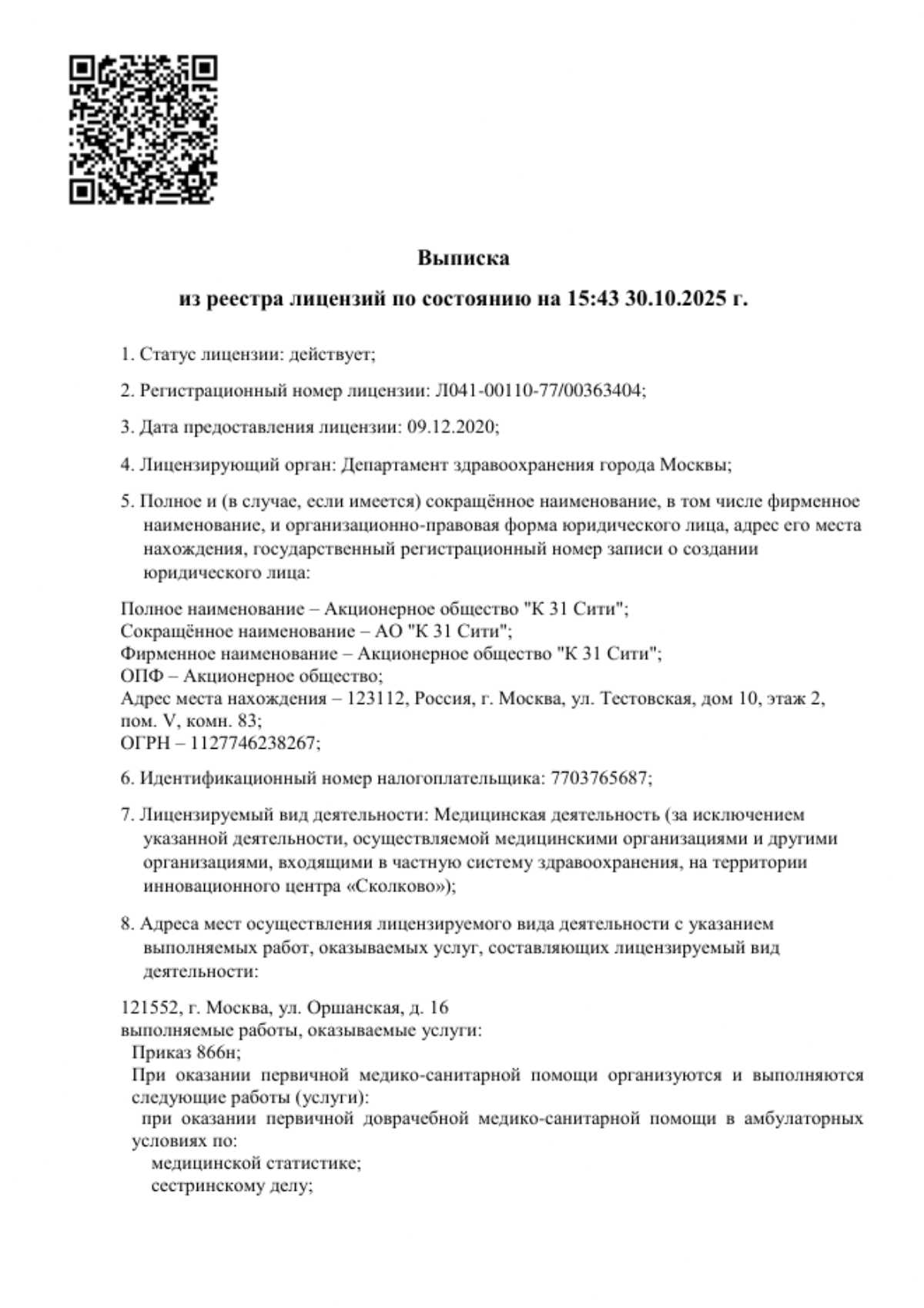
If you are looking for high-quality treatment for a growth using advanced, gentle technologies, we recommend contacting the K+31 clinic. Our team consists of true professionals who utilize the latest diagnostic and therapeutic methods. Finding an approximate treatment price is easy: just call the clinic or download the price list from the center's website.
Questions and Answers
Does the lump always hurt?
No, some growths don't hurt at all. For example, a Bartholin's gland cyst is often not felt at all at first. However, a boil or herpes, on the other hand, immediately begins to cause discomfort.
If the formation is hard, does it mean it is cancer?
A hard lump in itself doesn't indicate anything bad, much less cancer. A doctor can determine the nature of the lump after an examination and the necessary tests. There's no need to panic prematurely.
How to treat a lump in the genital area at home?
Self-medication is dangerous and ineffective. For example, squeezing harmless growths like lipomas or sebaceous cysts is not recommended, as this can lead to infection. Only a doctor can make an accurate diagnosis and prescribe appropriate treatment. Before consulting a doctor, it's best to refrain from squeezing or treating the lump with inappropriate products.

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price
Other services



































































General information about lumps and growths
Pathological structures can arise from any type of tissue that makes up a woman's external genitalia: skin, subcutaneous tissue, muscle, lymphatic tissue, and blood vessels. Harmless growths and lumps grow slowly and remain confined to adjacent tissues.
Malignant tumors, on the other hand, progress rapidly, destructively invading nearby tissues and spreading daughter cells far beyond the primary lesion. Secondary lesions can develop in organs and lymph nodes distant from the genital area.