Hidradenitis axillaria treatment
Hidradenitis axillaria is a common condition that, without treatment, often becomes chronic, significantly reducing the patient's quality of life.
At our clinic, diagnosis and treatment are performed by specialists with extensive experience in dermatology and surgery. We use modern methods—from drug therapy to minimally invasive surgical interventions and laser treatment. This approach allows us to stop inflammation at an early stage, prevent complications, and achieve stable remission.
We tailor treatment individually, taking into account the stage of the disease and associated factors, ensuring maximum effectiveness and reducing the risk of relapse.

specialists

equipment

treatment

Causes and risk factors
Hidradenitis suppurativa develops due to blockage of sweat gland ducts and subsequent inflammation. However, the exact mechanism of the disease is more complex: it is a combination of hereditary, immune, and external factors.
The main causes of hidradenitis suppurativa under the arm:
- Hyperkeratosis: skin cells around the duct actively grow and block it.
- Bacterial proliferation: microorganisms (most often Staphylococcus aureus and streptococci) begin to develop in the blocked gland.
- Immune response: the body reacts with inflammation, forming purulent lesions.
A combination of external and internal factors contributes to the development of hidradenitis suppurativa. Taking these factors into account is important for prevention and the correct choice of treatment.
Risk factors:
- Smoking: Nicotine increases inflammation and impairs the immune system
- Obesity: Excess weight increases skin friction and stimulates sweating, which creates favorable conditions for inflammation
- Hormonal imbalances: The disease is more common in women of reproductive age. Exacerbations are often associated with the menstrual cycle.
- Genetic predisposition: 30–40% of patients have a family history of the disease.
- Stress: Chronic tension affects hormonal levels and immunity.
- Microtrauma to the skin: Tight clothing, hair removal, and harsh deodorants increase the risk of inflammation.
The combination of several factors dramatically increases the likelihood of developing the disease.

Prevalence of hidradenitis
According to the WHO, hidradenitis occurs in 1–4% of the population. These figures may be underestimated, as the disease is often diagnosed in its late stages or confused with boils.
Women are affected 2–3 times more often than men. The disease most often occurs in young patients aged 18–35. After age 50, the risk decreases, which is associated with hormonal changes and decreased sweat gland activity. Hidradenitis is more common in countries with high obesity rates.

Symptoms and pathogenesis
Hidradenitis develops gradually, so it is important to recognize the first signs to begin treatment as early as possible and prevent complications.
Initial symptoms of the disease:
- A small, painful nodule under the skin in the armpit
- Mild itching or discomfort
- Redness of the skin
As the nodule progresses, it enlarges, becomes firm, and painful. The skin over the lesion becomes red, swollen, and an abscess forms, which may rupture on its own.
The chronic stage is accompanied by the formation of fistula tracts, scarring, and thickening of the skin. In severe cases, the process can involve the entire axilla, limiting arm movement.
Some patients experience fever, weakness, and enlarged regional lymph nodes. This indicates more severe inflammation and requires systemic treatment.
Hidradenitis is classified as an immune-inflammatory disease. Its development involves several stages:
- Duct obstruction. Increased keratin production and changes in sweat composition lead to blockage of the glandular duct.
- Microbial proliferation. The obstructed gland becomes an ideal breeding ground for bacteria, most commonly Staphylococcus aureus, Streptococcus pyogenes, and gram-negative bacteria.
- Immune response. T-lymphocytes and cytokines (tumor necrosis factor-alpha, interleukins) are activated, causing inflammation and tissue destruction.
- Chronic course. The inflammatory process persists, leading to the recurrence of nodules, sinus tracts, and cicatricial deformities.
Modern research shows that hidradenitis is not just an infection, but a systemic skin disease with a disrupted immune response. Therefore, the disease requires a careful, comprehensive approach.
Diagnosis of hidradenitis
The diagnosis is most often made based on a visual medical examination. The doctor determines when the nodules first appeared, the frequency of recurrences, and whether there are any relatives with similar symptoms. During the examination, the specialist assesses the number and extent of the nodules, as well as the presence of abscesses, fistulas, and scars.
Assessing hidradenitis according to the Hurley classification helps determine the optimal treatment strategy. To determine the stage of the disease and rule out other conditions, doctors use laboratory and instrumental methods.
Laboratory diagnosis
If hidradenitis suppurativa is suspected, the following laboratory tests are prescribed:
- Complete blood count: during an exacerbation, elevated white blood cells and ESR are detected.
- C-reactive protein: a marker of systemic inflammation.
- Bacteriological culture of discharge: helps identify the pathogen and its sensitivity to antibiotics, which is especially important in cases of frequent relapses or the ineffectiveness of standard therapy.
- Hormonal profile: sometimes prescribed to women if hormonal imbalances are suspected.
Instrumental diagnostics
To clarify the diagnosis and determine treatment options, the doctor may prescribe instrumental examinations:
- Soft tissue ultrasound: helps determine the depth and extent of inflammation and identify hidden abscesses. This is a safe and accessible examination method that can be performed without restrictions.
- MRI: used in severe chronic cases with multiple fistula tracts. The data obtained during the examination helps the surgeon plan the operation.
- Dermatoscopy: used to assess the skin condition and differentiate it from other diseases.
Differential diagnosis
To establish a diagnosis, it is important to conduct a differential diagnosis and distinguish hidradenitis from other conditions:
- Furuncle: acute inflammation of the hair follicle with the formation of a purulent core. The process is usually solitary, resolves more quickly, and recurs less frequently than hidradenitis.
- Lymphadenitis: inflammation of a lymph node, usually accompanied by a systemic infection. The node is enlarged and painful, and the skin over it may become red.
- Soft tissue abscess: a localized collection of pus in the subcutaneous tissue. Develops primarily after trauma, puncture, or injection.
- Tuberculosis of the skin: a chronic disease that causes fistulas and dense nodules. The pathological process is characterized by slow development and a prolonged course.
- Tumors of the skin and subcutaneous tissue: in rare cases, malignant neoplasms (e.g., squamous cell carcinoma) can mimic chronic hidradenitis, especially with long-standing or atypical nodules.
Accurate diagnosis of hidradenitis is especially important in the early stages to select effective treatment and prevent the disease from progressing to a severe form.
Complications of hidradenitis

If the disease is treated only at the abscess stage, but relapses are not controlled, complications develop over time:
- Chronic fistulas: channels connecting the site of inflammation to the skin surface that secrete pus, heal poorly, and are prone to recurrence.
- Scars: occur as a result of constant inflammation and tissue healing. They can not only cause aesthetic discomfort but also limit hand mobility.
- Extensive infiltrates: a complication in which several lesions merge into a single inflamed area.
- Lymphostasis: lymphatic stagnation leading to swelling of the arm. Occurs when the lymphatic vessels are damaged.
- Sepsis: a life-threatening condition in which bacteria from the lesion enter the bloodstream and cause a generalized infection. Occurs in rare cases.
- Anemia of chronic inflammation: with prolonged inflammation, hemoglobin levels in the blood can decrease significantly.
- Psychological issues: with advanced disease, patients may suffer from depression and social isolation.
Squamous cell carcinoma of the skin is a rare but possible complication of hidradenitis suppurativa. The risk of malignant transformation increases with prolonged disease progression—more than 20 years, especially if multiple fistulas develop. If dense or non-healing nodules appear, the fistula pattern changes, bleeding, or ulcers develop, a biopsy is necessary to rule out cancer.
Hidradenitis treatment
Conservative treatment
In the early stages of the disease and in uncomplicated cases of hidradenitis suppurativa, the following conservative treatments are prescribed:
- Antibiotic therapy: for mild cases, topical antibiotics; for moderate and severe cases, systemic antibiotics. Long courses of antibiotics (up to 10-12 weeks) are indicated for frequent relapses.
- Anti-inflammatory therapy: nonsteroidal agents that reduce pain and swelling. In cases of severe inflammation, short courses of systemic glucocorticosteroids are sometimes prescribed.
- Biologics: For severe cases of antibiotic-resistant hidradenitis suppurativa, TNF-α inhibitors are used, which reduce the activity of the immune response and reduce the frequency of relapses.
- Hormone therapy: Prescribed for women with flare-ups dependent on the menstrual cycle.
- Local antiseptics: Reduce the bacterial load and decrease the risk of new nodule formation.
- Physiotherapy: Laser therapy and photodynamic therapy can reduce inflammation. These methods are used only as adjunctive measures.
It is also important for patients with hidradenitis suppurativa to make lifestyle changes: quit smoking, use safe deodorants, and choose comfortable cotton clothing.
Surgical treatment
Surgery is indicated for chronic and severe cases when conservative therapy is ineffective.
Surgical options:
- Abscess drainage is performed during acute inflammation with severe pain and pus accumulation. The procedure quickly alleviates the condition but does not prevent further exacerbations, so it is often considered a temporary measure.
- Fistula excision: indicated for chronic inflammation with the formation of individual fistula tracts. The doctor removes the inflamed tissue along with the tracts, which reduces the risk of recurrence, but does not completely eliminate it.
- Wide excision: used for long-term recurrent inflammation, multiple lesions, and extensive skin lesions. The surgeon removes the entire affected area along with the subcutaneous tissue. Skin grafting is sometimes required after surgery. This is the most radical method, significantly reducing the likelihood of recurrence.
- Laser removal: used for limited lesions or fistula tracts. The laser allows for targeted removal of affected tissue with minimal trauma to the surrounding skin. This method produces good cosmetic results and has a short recovery period.
Treatment by stage
Treatment for hidradenitis suppurativa depends on the stage of the disease. In stage I, topical treatments are sufficient: antibiotics in the form of ointments or creams, as well as antiseptics for skin treatment. The goal of therapy is to stop the inflammation and prevent purulent formation.
In stage II, when the nodes become multiple and fistulas and purulent cavities may form, topical treatments alone are no longer sufficient. The doctor prescribes systemic antibiotics, as well as physiotherapy methods (such as UHF or laser therapy), which reduce inflammation and accelerate healing. Surgical excision is possible for isolated recurrent lesions.
In stage III, the disease becomes chronic: multiple fistulas, indurations, and scars appear. In such cases, biological therapy (TNF-α inhibitors and other modern drugs) is used, as well as radical surgical removal of the affected tissue, often followed by plastic surgery.
FAQ
Can hidradenitis suppurativa be treated at home?
No. Folk remedies and warm compresses can only worsen the condition. Effective treatment includes antibiotics, surgery, or biological therapy.
Is hidradenitis suppurativa contagious?
No. It is not infectious. The inflammation is related to the skin's natural characteristics and immune response, not to direct bacterial transmission.
Do ointments and creams help?
Topical antibiotics can be helpful in the early stages, but in chronic cases, ointments alone are insufficient. Therefore, any medications should only be used as prescribed by a doctor.
Is it okay to exercise?
Yes, physical activity is beneficial. The main thing is to avoid excessive friction and overheating. It's best to choose loose clothing and breathable fabrics.
Is it possible to be completely cured?
Yes, especially if the disease is diagnosed at stage I. In chronic cases, the goal of treatment is not a complete cure, but rather control of the disease and reduction of relapses.
Is hidradenitis suppurativa life-threatening?
In rare cases, severe complications, including sepsis or skin cancer, are possible. However, with modern treatment, the risk of serious health complications is minimal.

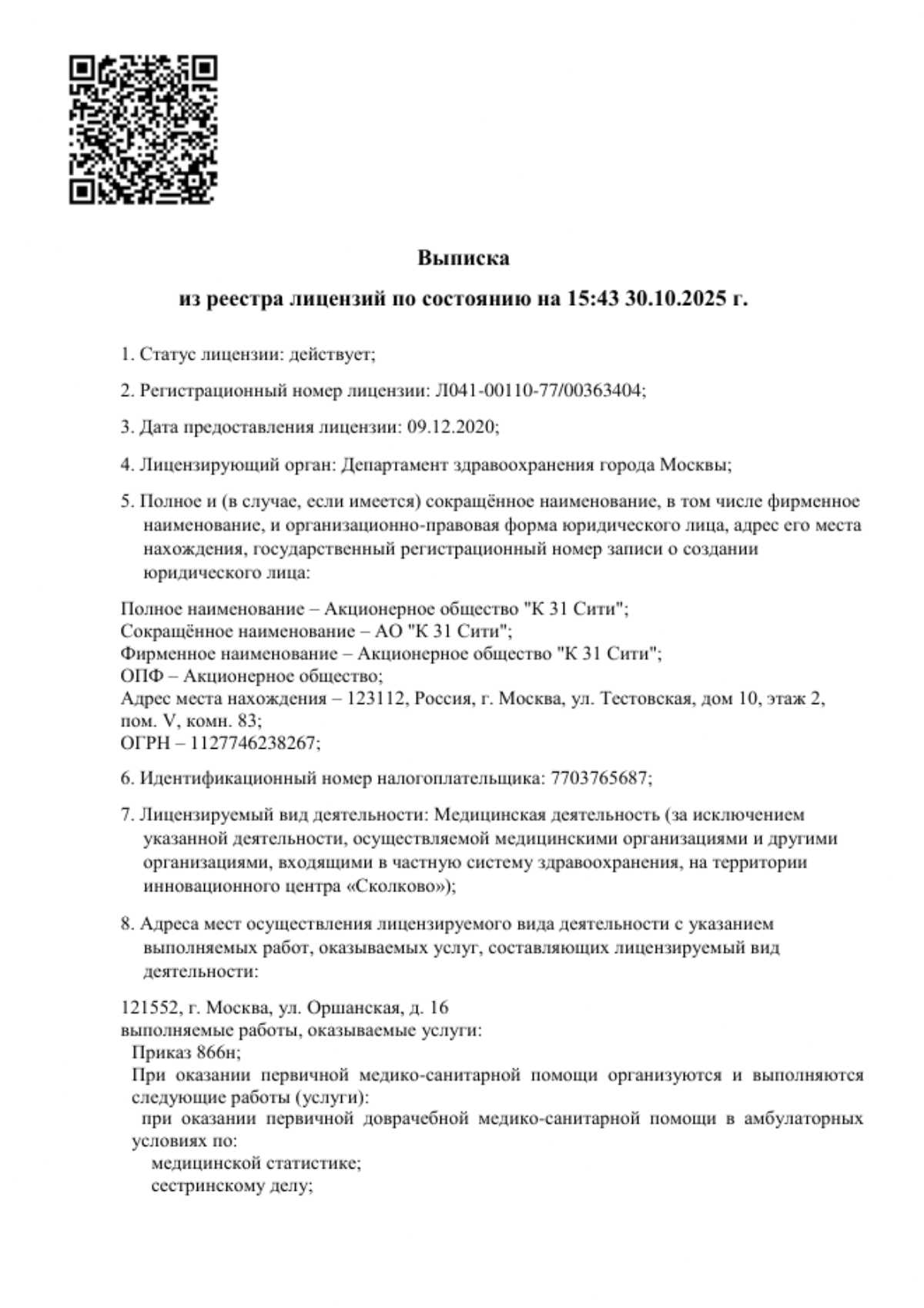
This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price
Other services




































































Definition and classification
Hidradenitis is a chronic skin inflammation associated with damage to the sweat glands. The classic form of the disease manifests as axillary abscesses, but inflammation can also occur in the groin, buttocks, and submammary folds.
The main characteristic of the disease is its recurrence. Nodules and fistulas reappear even after treatment. The disease belongs to a group of chronic skin inflammations and can significantly reduce quality of life: it interferes with movement, causes pain, and leads to psychological problems.
To determine the severity of the disease, modern doctors use the Hurley classification: