Herniated disc treatment
Herniated disc is a condition characterized by displacement and protrusion of the nucleus pulposus of the intervertebral disc beyond its anatomical limits. This condition is characterized by intense pain, numbness in the extremities, and limited mobility, significantly reducing the patient's quality of life.
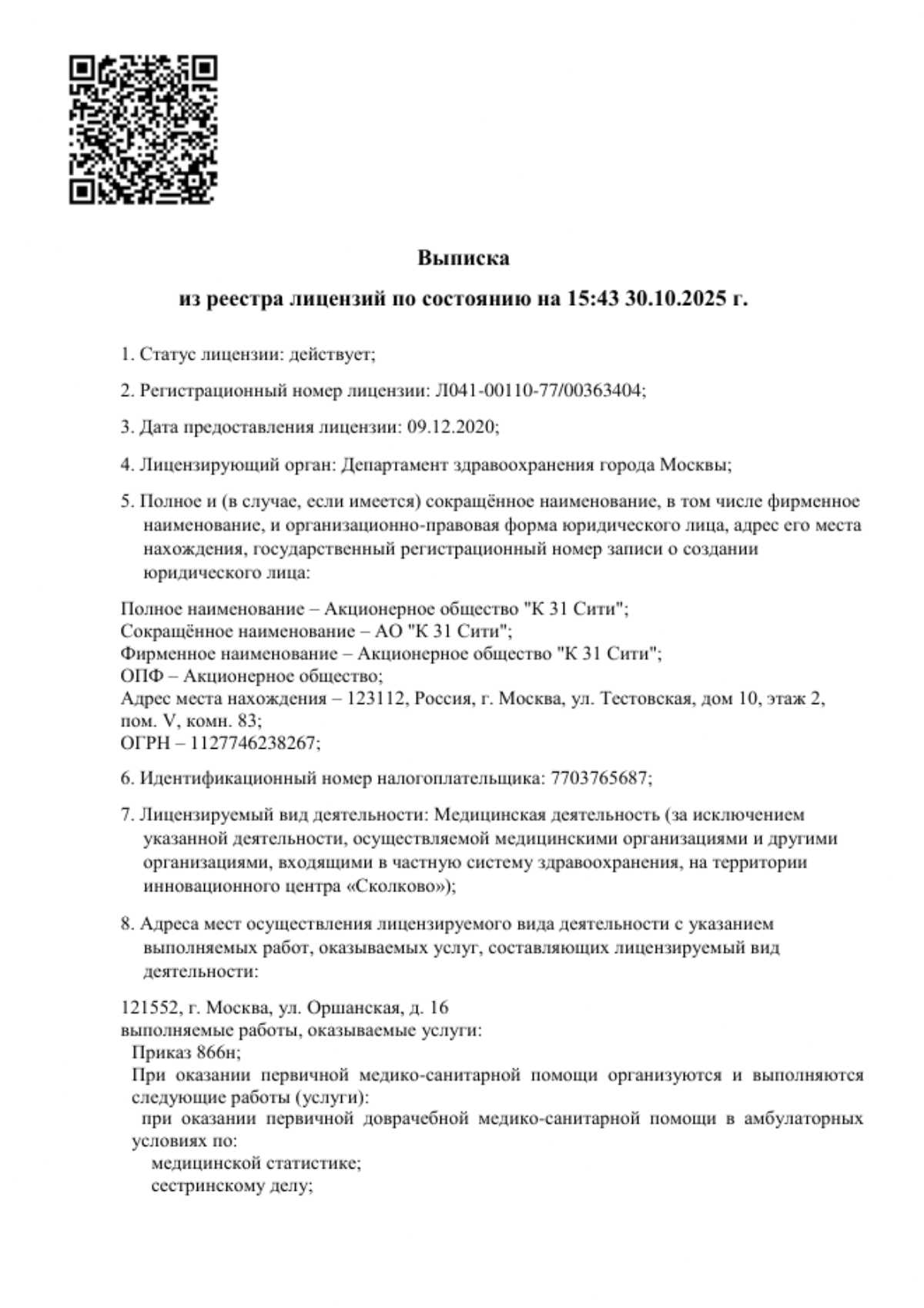
Modern medicine offers a comprehensive approach to herniated disc treatment, ranging from effective conservative methods to innovative surgical interventions. The K+31 Clinic in Moscow utilizes advanced treatment protocols, including physiotherapy, exercise therapy, and, if necessary, modern surgical procedures aimed at rapid patient recovery.
Individually tailored, timely treatment helps relieve symptoms, prevent complications, and ensure a pain-free return to an active life.

specialists

equipment

treatment
Causes and main risk factors
Causes of herniation
Proximate causes can be considered triggers that initiate the process of disc herniation against the background of existing destructive changes in the tissue. These include:
- Disc degeneration. With age or metabolic disorders, the intervertebral disc loses moisture and the substances dissolved in it. The nucleus pulposus dries out, losing its shock-absorbing properties, and the fibrous ring becomes more fragile and covered with microcracks. A weakened disc cannot withstand even normal loads, which ultimately leads to its bulging.
- Excessive strain. Lifting heavy objects, especially while bending and twisting the torso, creates tremendous pressure. The weakened fibrous ring cannot withstand this and ruptures. This is how disc herniations often occur in people who are not accustomed to systematic physical activity.
- Trauma. Direct trauma, such as a fall on the back, a blow, or a neck injury, can immediately damage a disc and directly cause a herniated disc.
- Weakness of the muscular framework. The back and abdominal muscles normally create a natural support system for the spine. When they are weak, the entire load falls directly on the vertebrae and intervertebral discs, accelerating wear and degeneration.
Risk factors
These factors cannot be considered a direct cause of pathology, but they significantly increase the likelihood of developing the disease:
- Age – the natural aging process invariably affects the condition of all tissues, including cartilage, muscle, and bone.
- Sedentary work – prolonged immobility leads to impaired blood flow and weakens muscles or, conversely, leads to hypertonicity due to tension.
- Overweight – obesity creates constant additional stress, causing disc subsidence and destruction.
- Inadequate physical activity – weightlifting without proper technique, sudden twisting movements, and work involving heavy lifting systematically injure discs.
- Genetics – a hereditary predisposition can determine the structural features of connective tissue and metabolism, affecting the strength of fibrous discs. rings
- Pregnancy – due to the growing belly, the center of gravity shifts and the load on the spinal column is distributed incorrectly, and relaxin, released to soften the ligaments of the pubic symphysis, also affects the connective tissue of the spine, making it more vulnerable to damage.

Clinical picture of the disease
The symptoms of a herniated disc are directly related to its impact on the surrounding nerve structures. The main cause of symptoms is mechanical compression. This leads to three groups of symptoms: pain, neurological deficit, and muscle tension.
Main signs
Symptoms are most pronounced in the area where the disc protruded. Initially, the pain is aching and intensifies with movement and stress. As the disease progresses, the pain begins to spread along the main nerve fibers and radiate to other areas.
Other, less specific symptoms may also be of concern:
- Lasegue's symptom, or tension symptom – the occurrence of sharp pain in the lower back and along the sciatic nerve when raising a straight leg while lying down, and its disappearance when bending the knee.
- Sensory disturbances
- Muscle weakness
- Autonomic dysfunction – a feeling of chills or heat without significant fluctuations in body temperature, increased sweating, dry skin.
Characteristics of pain syndrome
Pain from a herniated disc is varied and usually has several mechanisms of occurrence:
- Localized pain. Aching, deep. It is associated with irritation of pain receptors in damaged spinal structures.
- Radicular pain. Sharp, shooting, burning, piercing. It occurs directly due to compression of a nerve root. It follows the innervation of the damaged nerve.
Pain may increase sharply with coughing, sneezing, straining, as well as with bending, sitting, or standing for long periods.
Differences depending on location
The location of the hernia determines which nerve structures are compressed and, accordingly, affects the overall clinical picture.
If the lumbar spine is affected, the patient, in addition to the main symptoms, may experience:
- Leg pain
- Numbness down to the toes
- Foot weakness
- Inability to sit or stand on tiptoes
- Unsteady gait
A herniated disc in the cervical spine may cause:
- Neck pain radiating to the shoulder blade, shoulder, and down the arm to the fingers
- Pain in the occipital region
- Dizziness, tinnitus accompanied by fluctuations in blood pressure
- Numbness and weakness
Symptoms that may indicate a thoracic bulge include:
- Intercostal neuralgia – a girdle-like pain along the ribs that intensifies with deep inhalation, coughing, and torso rotation.
- Pain that mimics internal organ diseases: cardialgia, pain in the stomach or pancreas.
- Numbness in the chest or abdomen.

Development of pathology
The process of disc herniation usually begins with a disruption in the diffuse nutrition of the intervertebral discs, which in adults lack their own blood vessels and receive moisture and nutrients from surrounding tissues through osmosis.
Aging, a sedentary lifestyle, or excessive stress disrupt metabolism in the disc. The nucleus pulposus loses water and proteoglycans, leading to decreased turgor and impaired shock-absorbing function. Simultaneously, radial cracks and areas of weakness develop in the structure of the annulus fibrosus due to repeated microtrauma and impaired collagen synthesis.
As the disc degenerates, it no longer evenly distributes axial load. The weakened annulus fibrosus cannot withstand the pressure of the displaced nucleus pulposus and ruptures. Through the resulting defect, fragments of the nucleus pulposus protrude beyond the disc, forming a herniated protrusion.
The main pathological effect is not only mechanical compression of the nerve. The prolapsed nucleus, being foreign to the immune system, often causes irritation and aseptic inflammation, leading to localized swelling, impaired blood circulation in the nerve, and the development of intense pain.

Classification and stages of development
Based on their anatomical location relative to the center of the spinal canal, there are four types of herniated discs:
- Median – located centrally, along the midline, can compress spinal cord structures.
- Paramedian, or lateral – located to the side of the midline, most often causes nerve root compression.
- Foraminal – located in the narrow intervertebral foramen where the nerve root emerges, causing significant compression even at a small size.
- Posterior, or dorsal – directed toward the spinal cord.
A herniated disc goes through four stages in its development, each with its own characteristics.
- Degeneration. This is the stage of preliminary destructive changes in the tissues without the formation of a bulge.
- Protrusion. The annulus fibrosus weakens and cracks appear, but the integrity of the outer layers is maintained. The nucleus pulposus shifts, causing a disc bulge. This is not yet a herniation, but often precedes one.
- Extrusion. The fibrous tissue is destroyed. The nucleus pulposus shifts but remains attached to the disc. This bulge can then compress a nerve root or the dural sac.
- Sequestration. A fragment of the nucleus pulposus completely separates from the disc and enters the spinal canal, causing intense inflammation.

Possible Complications
Failure to promptly treat a herniated disc can lead to complications, many of which are irreversible. The main cause of these complications is progressive damage to nerve tissue due to prolonged compression and inflammation.
Radicular syndrome, or radiculopathy, is the most common complication. This is not a single disease, but a complex of symptoms that occur when a spinal nerve is compressed. It manifests as sharp, shooting pain along the nerve, numbness, tingling, and muscle weakness in the area it innervates.
Untreated radiculopathy can result in paresis and muscle atrophy. Constant compression of the motor nerve fibers disrupts the transmission of impulses from the spinal cord to the muscles, leading to muscle weakness. A patient with a lumbar disc herniation may have difficulty standing on their toes or heels, or raising their arm with a cervical disc herniation. Long-term disruption of innervation causes muscle atrophy. Muscles shrink, lose strength, and can no longer fully perform their functions, significantly limiting mobility.
Spinal segment instability is a complication that develops after significant disc degeneration. Having lost its height and elasticity, the intervertebral disc no longer reliably stabilizes the two adjacent vertebrae. They become abnormally mobile, placing excessive strain on the muscles and ligaments, causing chronic pain and the risk of developing spondylolisthesis. This condition often requires surgery with the placement of stabilizing devices.
Some complications are life-threatening and require emergency surgery. One such condition is cauda equina syndrome. It occurs when a massive central disc herniation compresses a bundle of nerve roots, resembling a horse's tail and located in the lower part of the spinal canal. Its symptoms include:
- Acute lower back pain radiating to both legs
- Perineal numbness
- Incontinence or, conversely, urinary and fecal retention
- Progressive weakness in the legs
If these symptoms appear, seek medical attention immediately, as delay can lead to irreversible paralysis and disability.
Diagnostic methods

Diagnosis begins with a consultation with a neurologist. The specialist interviews the patient, determining the nature of the pain, its location, radiation, and any factors that may be causing it to worsen.
A neurological examination is important. During this examination, the doctor checks for:
- Tendon reflexes (knee, Achilles) – their decrease or absence indicates compression of a specific nerve root.
- Muscle strength and tone – weakness of specific muscles is detected.
- Sensation – the presence of numbness or hypoesthesia is checked.
- Specific tension symptoms – their presence confirms nerve root compression and helps differentiate a herniated disc from a muscle spasm.
After this stage, the doctor formulates a preliminary diagnosis and refers the patient for further instrumental examination, which will help determine the stage of the pathological process and choose an effective treatment strategy.

MRI is considered the gold standard for diagnostics. Only this method accurately:
- Visualize the intervertebral disc itself, assess its condition, height, and degree of degeneration.
- See the size, location, and direction of the protrusion.
- Assess the degree of compression of the nerve endings.
- Detect sequestration.
- Differentiate herniation from other conditions, such as a tumor or hemangioma.
In cases where MRI is impossible due to absolute contraindications, such as a pacemaker or metal implants in the imaging area, computed tomography is used. CT scans are good at visualizing the bony structures of the vertebrae, but are significantly inferior to MRI in assessing the condition of the discs themselves and surrounding tissues.
Spinal X-rays cannot detect a herniated disc because they do not visualize soft tissue. However, this method plays an important adjunctive role. It is prescribed to rule out other causes of pain, such as fractures, vertebral displacement, or bone infections, as well as for a general assessment of the spinal anatomy to detect signs of osteochondrosis, curvature, and instability.
Treatment methods
Conservative therapy
Conservative treatment is the primary approach for most patients (approximately 80-90% of cases). Its goals are to relieve pain and inflammation, relieve muscle spasms, support the muscular corset to stabilize the spine, and prevent recurrence. It is indicated for small and medium-sized herniated discs without threatening neurological complications.
Non-drug methods
This is the basis of conservative treatment, aimed at improving biomechanics and activating the body's own regenerative resources.
The following may be helpful:
- Physical therapy. Exercises strengthen the back and abdominal muscles, which form a natural corset, reducing stress on the disc.
- Massage. Relaxes tense muscles, improves blood circulation and lymph flow in the affected area.
- Physiotherapy. Helps reduce pain, eliminate swelling, suppress inflammation, and initiate regenerative processes. Modern methods are used: laser therapy, ultrasound therapy.
- Traction therapy – spinal traction. Used with extreme caution and only as prescribed by a doctor to increase intervertebral space and reduce pressure on the nerve root.
- Kinesio taping. The application of elastic bands is recommended to support muscles and reduce strain without limiting movement.
Drug therapy
Used for the rapid relief of acute symptoms. The doctor may prescribe:
- Nonsteroidal anti-inflammatory drugs
- Muscle relaxants
- B vitamins
For severe pain that is not relieved by topical and systemic medications, therapeutic nerve blocks are administered. This procedure involves injecting a local anesthetic, often with a corticosteroid, directly into the inflammation around the pinched nerve.
Surgical treatment
Surgery for a spinal disc herniation is recommended only when all conservative treatment options have been exhausted or when urgent intervention is initially indicated.
Surgical methods are resorted to in the following conditions:
- Ineffectiveness of conservative therapy within 4-6 weeks with severe pain
- Cauda equina syndrome
- Increasing paresis in a limb
- Progression of muscular atrophy
- Large sequestered disc herniation
Surgical options
Modern surgery offers patients procedures performed using minimally invasive techniques. This approach allows for the herniation to be eliminated, restoring spinal health with minimal damage to healthy tissue and a shortened rehabilitation period.
- Endoscopic discectomy. The herniation is performed through a minimal incision (less than 1 cm) using an endoscope that transmits the image to a monitor.
- Microdiscectomy. The surgery is performed through a small incision (3-4 cm) using an operating microscope.
- Minimally invasive techniques. These include nucleoplasty, in which cold plasma or laser energy is delivered through a puncture needle into the disc, vaporizing part of the nucleus pulposus, reducing the size of the herniation and pressure on the nerve. Hydroplasty, which is performed similarly, but the nucleus pulposus is eroded and aspirated with a saline solution.
General information
FAQ
Can a herniated disc be heated?
During the acute phase of the disease, when severe pain is present, heating the affected area is strictly not recommended. Heat increases blood flow, which can lead to increased swelling around the pinched nerve root and a significant increase in pain. Heating is possible during the recovery phase of a spasm. In this case, dry heat is used in short courses.
Is surgery always necessary for a hernia?
No, the vast majority of patients do not require surgery. Surgical treatment is a last resort. Comprehensive conservative treatment (medications, nerve blocks, physical therapy, and exercise therapy) is used first. Surgery is considered only if such treatment is ineffective or complications arise.
How to sleep properly?
Proper sleeping position helps relieve pressure on the spine and reduce pain. Ideally, sleep on your back with a bolster under your knees to relax your lower back and keep it firmly in contact with the mattress. You can also sleep on your side in the fetal position. If you have pain on one side, lie on your healthy side. Pull your knees slightly toward your chest and place a small pillow between them. This aligns the pelvis and relieves tension. Sleeping on your stomach is not recommended, as it causes hyperextension in the lumbar spine and can worsen nerve compression.
Can I exercise?
Yes, but only after the acute pain has subsided. Complete abstinence weakens the muscles. Swimming, water aerobics, Nordic walking, therapeutic exercise, Pilates, and yoga are recommended. Running, jumping, weightlifting, martial arts, team sports with a high risk of injury, and any activity that causes pain are contraindicated. Consult your doctor before beginning any exercise program.
Bibliography
- Clinical Guidelines – Discogenic Lumbosacral Radiculopathy – 2023-2024-2025 (December 8, 2023) – Approved by the Russian Ministry of Health.
- Grin', A. A. "What is a Herniated Intervertebral Disc?" and Long-Term Results of Its Treatment // Neurosurgery. 2006. No. 3.
- Tolumbaeva, N. S. "Diagnosis and Treatment of Herniated Disc" // Vestnik AGIUV. 2011. No. 3.
- Dobysh A. A., Kirilenko S. I., Rozhin V. V., Mazurenko A. N. ANALYSIS OF THE RESULTS OF ENDOSCOPIC AND MICROSURGICAL REMOVAL OF LUMBAR DISC HERNIATIONS // Medical News. 2019. No. 7 (298).
- Sampiev M. T., Sychenikov B. A., Skabtsov N. V., Lyagin A. S., Rynkov I. P. Minimally invasive surgical treatment methods for lumbar disc herniation // Russian Medical Journal. Medical Review. Vol. 3, No. 7, 2019.

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price
Other services



































































Basic information about the pathology
An intervertebral disc, or intervertebral disc herniation, is a degenerative disorder of the spine in which a portion of a deformed intervertebral disc slips, causing compression of the nerve structures. To understand the nature of this pathology, it's important to understand the structure of the disc.
The intervertebral disc is a fibrocartilaginous structure that acts as a shock absorber between the vertebral bodies. It consists of two parts:
The process of disc herniation begins with gradual degeneration of the disc due to exposure to unfavorable factors.
The prevalence of this disease is quite high. According to medical statistics, up to 80% of adults aged 30 to 50 suffer from intervertebral disc herniations of various locations. The pathology most frequently occurs in the lumbar spine (over 65% of cases), as it is most susceptible to significant physical strain. The cervical spine accounts for approximately 30% of cases, and the thoracic spine accounts for no more than 5%.