Gastric bypass (gastric bypass)
Excess weight is not only an aesthetic concern but also a serious burden on the body, leading to shortness of breath, joint pain, hypertension, and diabetes. When diet and exercise fail to produce long-term results, surgery becomes an effective solution. Gastric bypass is a minimally invasive procedure that creates a small reservoir from the upper part of the stomach, connecting directly to the small intestine. This significantly reduces food intake and calorie absorption.
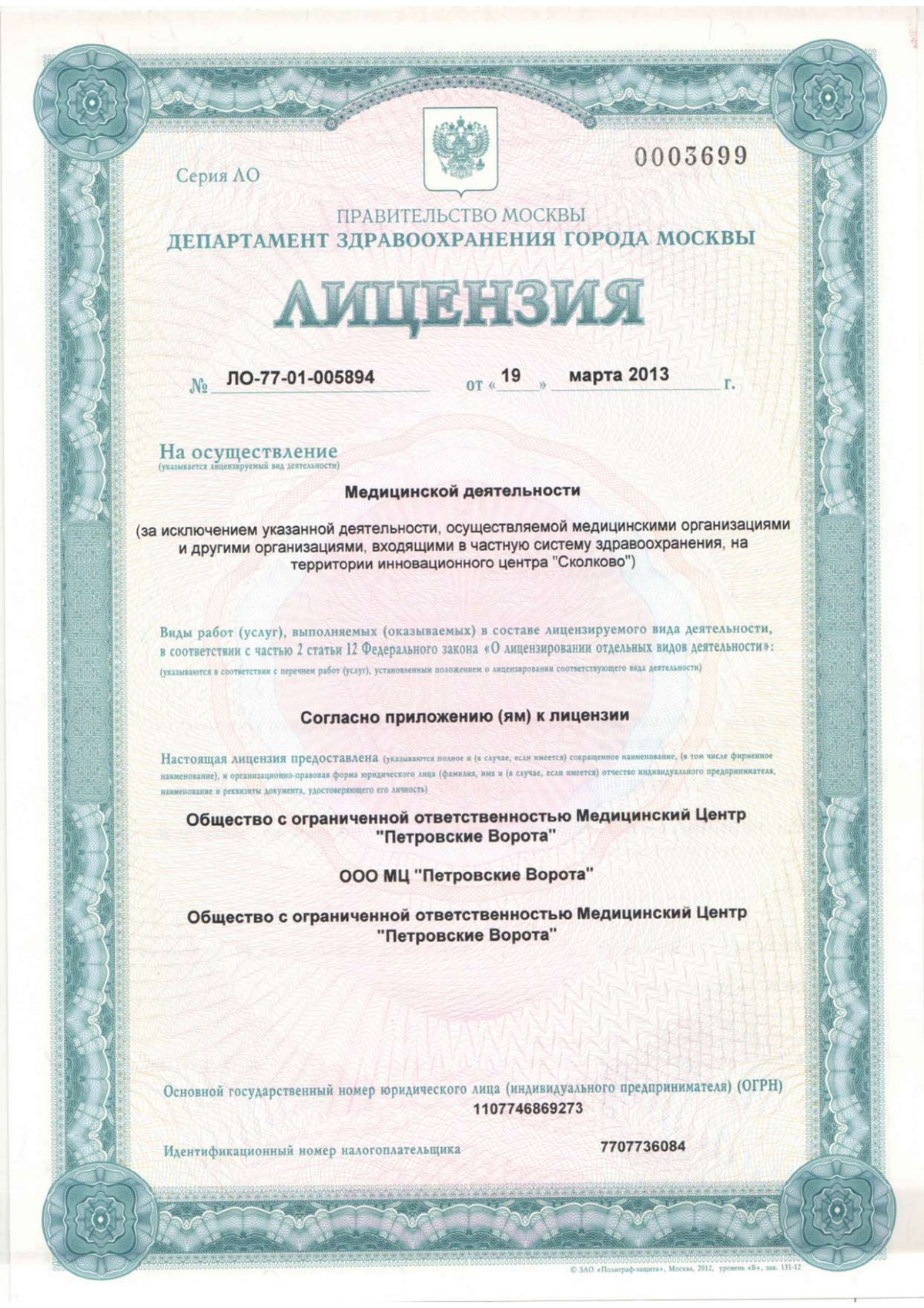
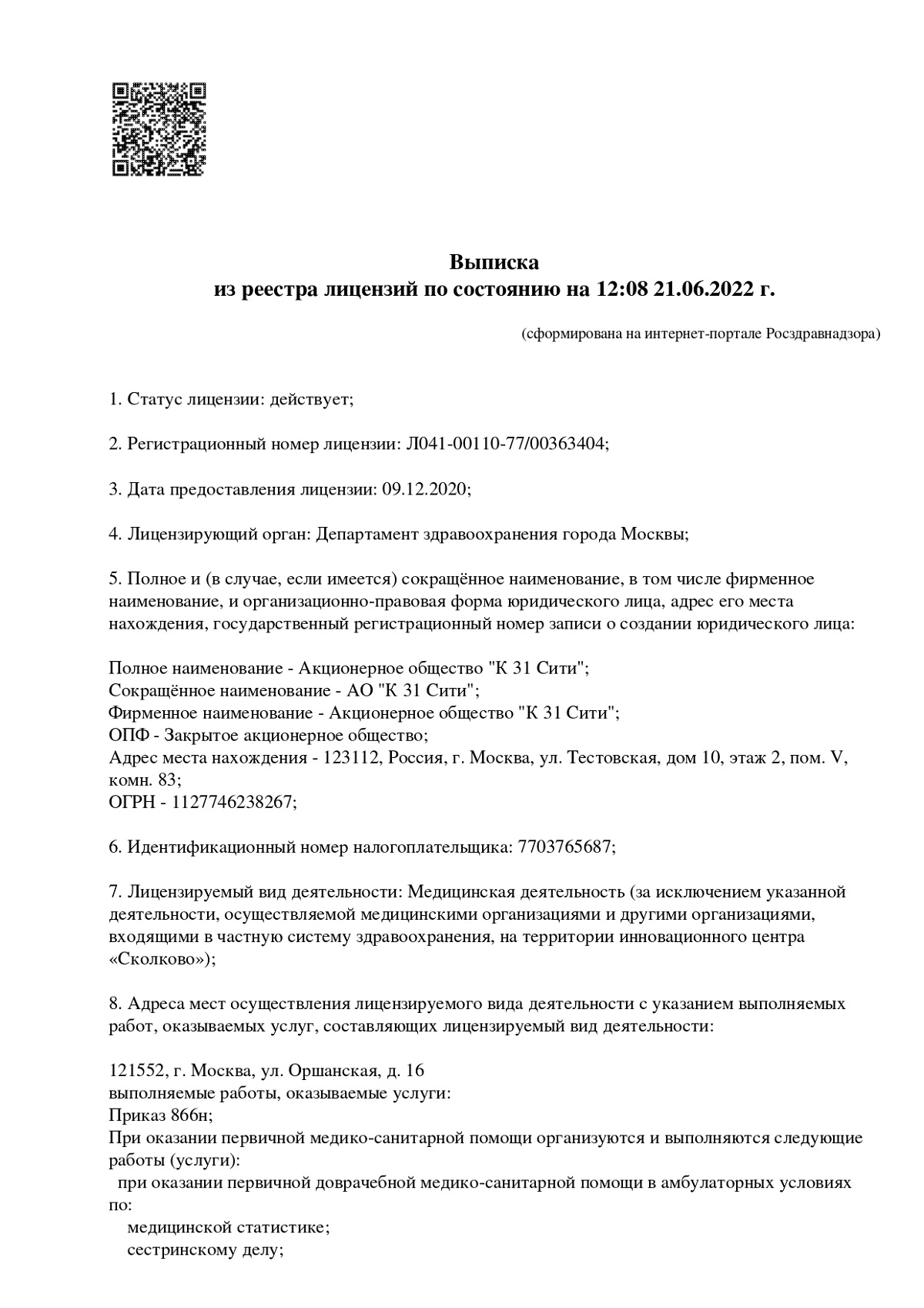
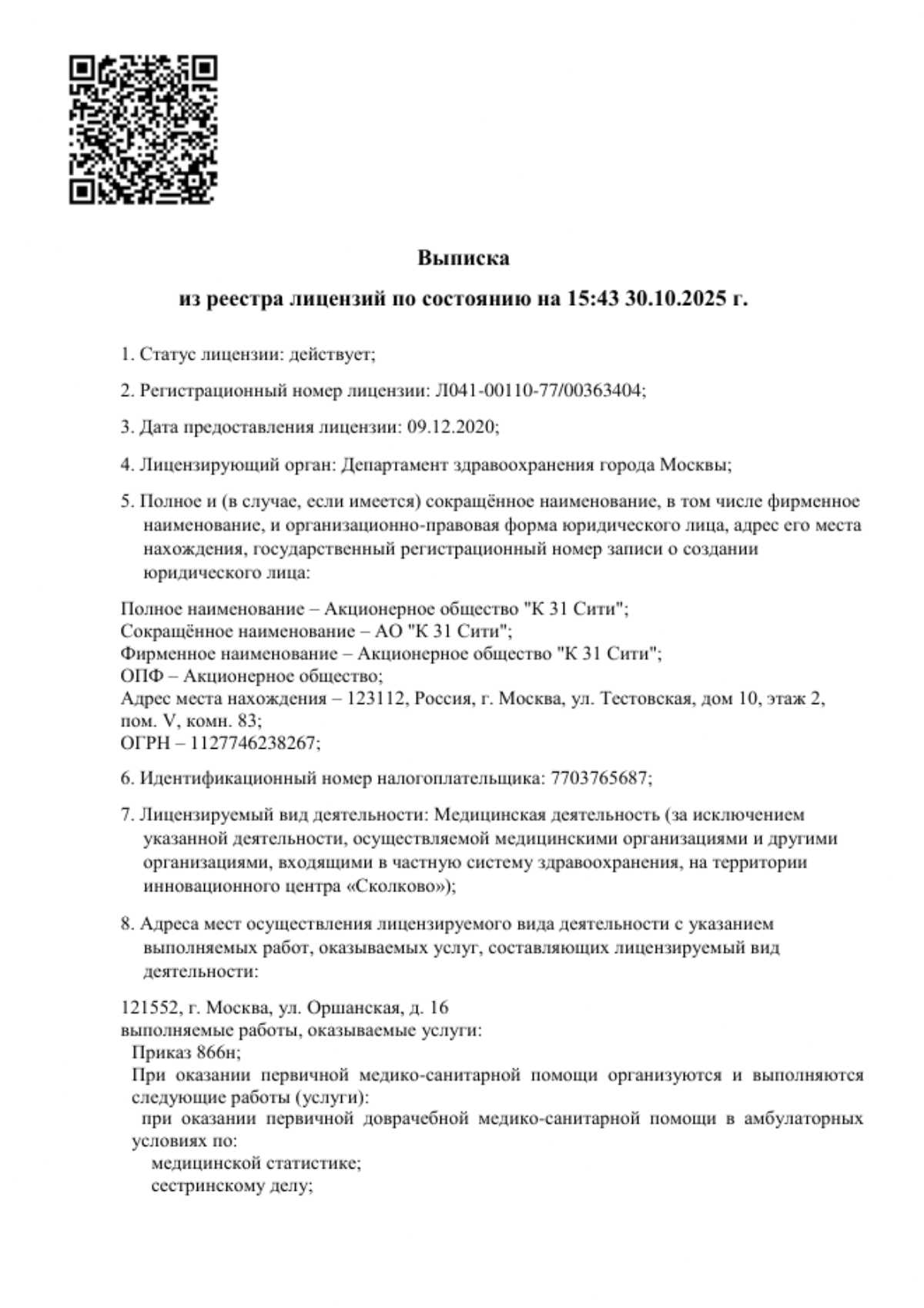
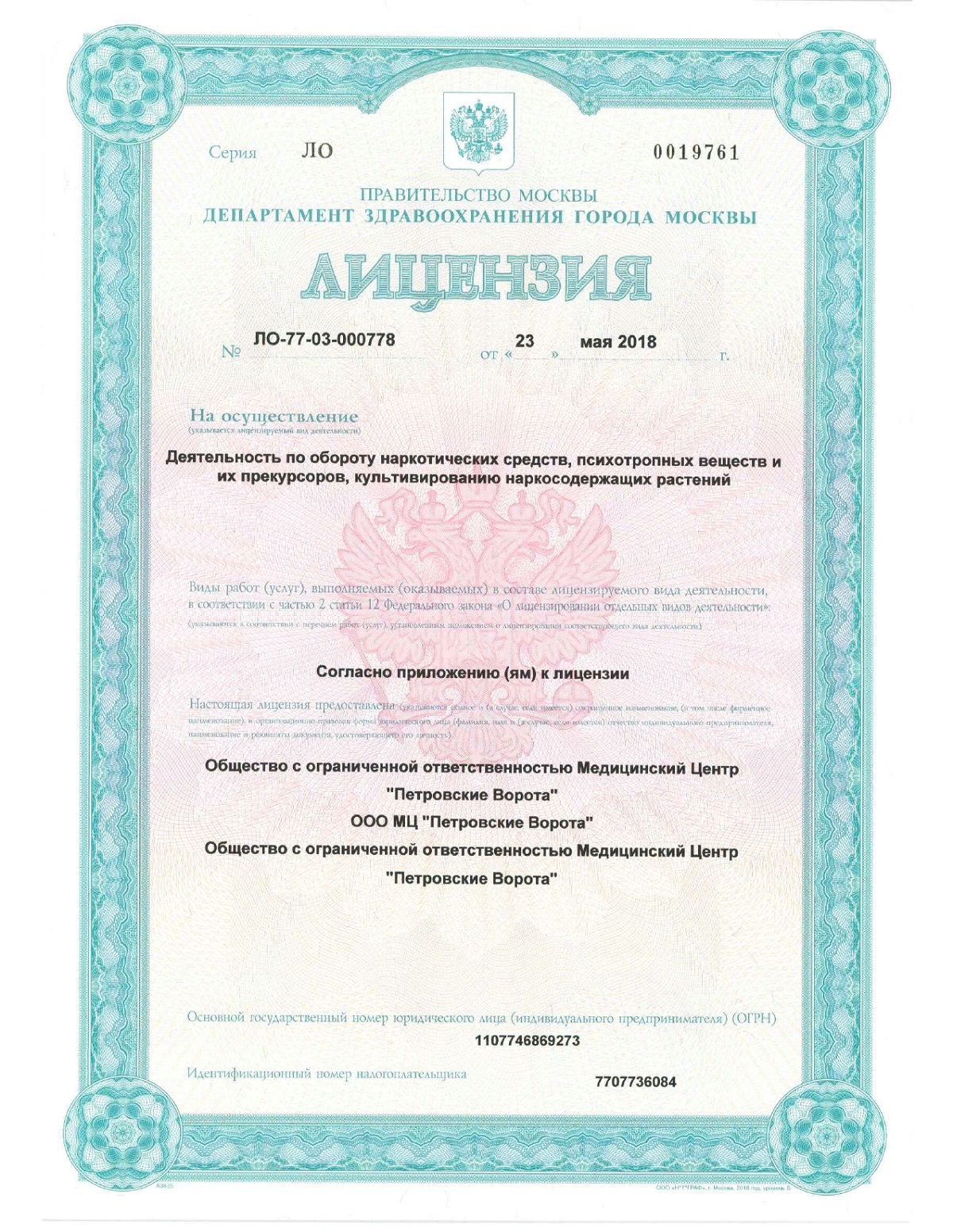
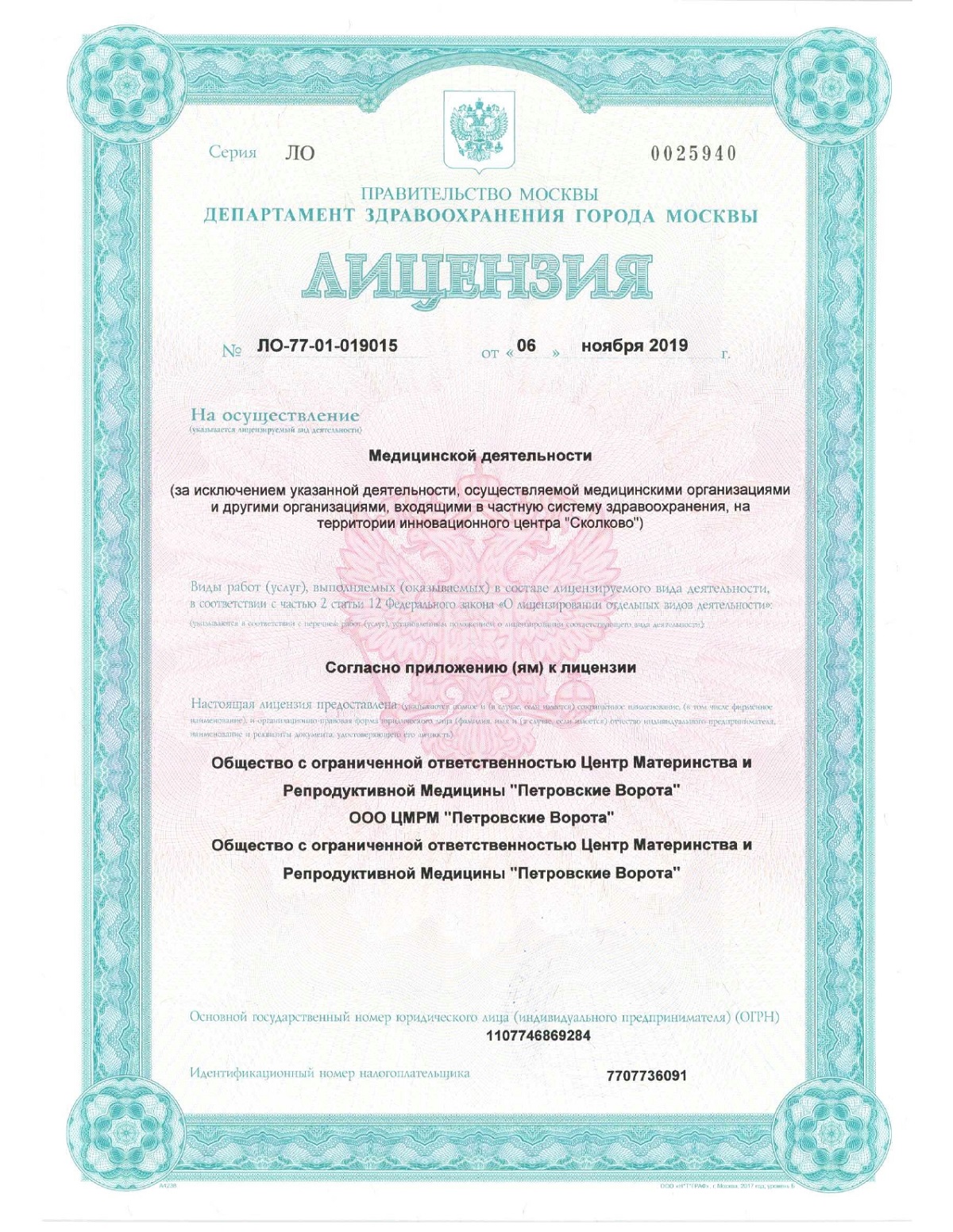
At the K+31 Clinic in Moscow, this procedure is performed using advanced laparoscopic technologies, ensuring minimal trauma and a quick recovery. We offer a comprehensive approach to obesity treatment, combining high-tech surgery, comfortable living conditions, and affordable pricing to help you return to a healthy and active life.

specialists

equipment

treatment

Who is indicated for surgery?
The decision to perform gastric bypass surgery is made collectively and based on strict medical criteria. It may be recommended when conservative methods of combating excess weight have exhausted their effectiveness.
Body mass index is a key marker for considering surgical correction. Surgery is recommended for patients diagnosed with morbid obesity, with a BMI exceeding 40. The procedure is also indicated for less severe but still severe obesity, with a BMI between 35 and 40, if accompanied by significant comorbidities. These include:
- Type 2 diabetes mellitus
- Resistant hypertension
- Obstructive sleep apnea syndrome
- Severe degenerative changes in the joints, significantly limiting mobility
It is important to understand that bypass surgery is not considered a radical alternative to diet and physical activity, but rather a necessary measure to preserve the patient's health and life when other methods have proven ineffective.

When an operation cannot be performed
Like any surgical procedure, gastric bypass has a number of limitations. All contraindications are divided into two categories: absolute, which completely preclude the possibility of surgery, and relative, which can be revised after eliminating the impeding factors.
Absolute contraindications include:
- Severe, uncompensated psychiatric disorders that prevent the patient from consciously following lifelong dietary and lifestyle recommendations.
- Oncological diseases.
- Severe irreversible dysfunction of the heart, liver, or kidneys.
- Acute inflammatory gastrointestinal diseases.
Relative, or temporary, contraindications require additional attention and preparation. These include circumstances such as young age, when the body has not yet fully developed, or the presence of bad habits that must be abandoned before surgery. Pregnancy and lactation also pose time limitations.
The presence of contraindications emphasizes the need for a comprehensive and thorough preoperative examination, the goal of which is to minimize risks and ensure long-term treatment success.
How to prepare for the intervention
Preparation in 2-3 months
During this period, the patient undergoes a comprehensive examination to identify any restrictions and subsequently address them. Their condition is monitored by a team of specialists.
Two to three months beforehand, the patient begins working with a nutritionist. The goal of this collaboration is to gradually change eating habits. At this stage, it is important to develop a mindful eating habit. Portion sizes are already reduced and calories are consumed. This helps normalize gastrointestinal function, significantly facilitating access to the stomach during surgery. After this preparation, the patient will be able to adapt to the new diet more easily.
If metabolic disorders are present, a consultation with an endocrinologist is mandatory. The doctor evaluates hormonal levels and corrects carbohydrate metabolism disorders. They also develop a diabetes management strategy, if the condition is diagnosed, to ensure stable levels by the time of surgery.
A consultation with a psychologist or psychotherapist is crucial to identify and address the psychological causes of overeating. The specialist also helps formulate reasonable expectations for the surgery and prepares patients mentally for the significant life changes that follow.
A comprehensive diagnostic examination is also performed. The standard protocol includes:
- gastroscopy to assess the condition of the gastric mucosa and rule out pathologies.
- ultrasound of the abdominal organs.
- a range of laboratory tests.
This allows for a complete picture of the patient's health and the elimination of hidden contraindications.
Preparation immediately before surgery
A few days before hospitalization, a low-residue diet is recommended. Avoid foods that cause fermentation and gas formation, such as raw vegetables, legumes, brown bread, and dairy products. Complete abstinence from food and liquid is required for 8-12 hours before the scheduled time to ensure complete evacuation of stomach contents.
Special attention is paid to adjusting medication therapy. It is important to discuss all medications, especially those affecting blood clotting, with your doctor and surgeon in advance. Their temporary discontinuation or replacement is strictly based on an individualized plan.
A mandatory final step is a consultation with an anesthesiologist. The specialist will thoroughly review your medical history and the results of all examinations, assess anesthetic risks, and select the optimal method of pain relief.
How does the operation proceed?
Gastrobypass is a high-tech procedure that is now performed using gentle techniques. Instead of a large incision, surgeons use a laparoscopic approach, making the procedure minimally invasive and significantly reducing the recovery period.
Stages
The procedure is performed in several sequential stages under general anesthesia.
- Creation of a laparoscopic approach. The surgeon makes several small punctures (usually 4-5 mini-incisions) in the anterior abdominal wall. Trocars—special tubes that serve as guides for a miniature video camera and long, thin instruments—are inserted through these incisions. The camera transmits a magnified, high-resolution image of the surgical area to a monitor.
- Creation of a small stomach. Using a special surgical apparatus, the upper part of the stomach is completely separated from the main, larger portion. This creates a small reservoir with a capacity of approximately 20-30 ml, which will function as a stomach, secreting gastric juice. The main part of the stomach is not removed, but is excluded from the food bolus's pathway.
- Creation of a digestive loop. The surgeon isolates a loop of small intestine and transects it approximately 1-1.5 meters from its origin. The lower end of this loop is brought to the newly created small stomach.
- Anastomosis—connection. This is the most crucial step. The surgeon creates a strong, watertight connection between the small stomach and the introduced loop of small intestine. Food will now flow directly into this new pathway.
- Restoring intestinal continuity. To prevent bile and digestive juices from the bypass (the remaining duodenum and the initial section of the jejunum) from being lost, the upper end of the isolated intestine is sutured to the newly created digestive loop below the gastrointestinal anastomosis. This creates a single pathway for food and digestive secretions.
- Suture placement. After hemostasis and sealing of the connections are verified, the instruments are removed, and cosmetic sutures are placed at the puncture sites.
Principles of modern surgical intervention
The key advantage of the modern approach is minimal invasiveness. Laparoscopic technique means that instead of extensive tissue trauma, only gentle penetration through small punctures occurs.
From a surgical perspective, the principle of operation is the creation of two circuits, providing both mechanical and metabolic action.
- The food loop is a shortcut through which food quickly passes from the small stomach to the intestine, providing early satiety and limiting calorie intake.
- The digestive loop is the pathway for bile and enzymes, which are mixed with food later, reducing the intensity of nutrient absorption.
Postoperative Risks
When deciding on gastric bypass, it is important to have complete and objective information not only about the benefits but also about the possible risks. The procedure, being extensive and technically complex even with a laparoscopic approach, is associated with a certain probability of complications, which are divided into general surgical and specific ones inherent to this type of surgery.
Dangers of Bypass: General Surgical Risks
Any surgical procedure performed under general anesthesia carries a standard set of potential risks. These include, first and foremost, an individual's reaction to anesthesia, the likelihood of which is minimized by the anesthesiologist's meticulous work during preoperative preparation.
In the early postoperative period, there is a risk of bleeding from the surgical site, as well as the formation of intravascular thrombi in the veins of the lower extremities. To prevent the latter, patients are actively encouraged to mobilize early and may be prescribed special anticoagulants. Furthermore, there is always a minimal risk of intra- and postoperative infection, damage to adjacent anatomical structures, and adhesion formation in the abdominal cavity.
Possible complications: specific risks of the technique
In addition to general risks, there are complications directly related to changes in the anatomy of the gastrointestinal tract.
- Anastomotic leakage. This is one of the most serious technical complications, in which a defect may develop in the area of the surgical suture, leading to the penetration of intestinal contents into the abdominal cavity. This situation requires immediate surgical intervention.
- Anastomotic stenosis. A cicatricial narrowing may form at the junction of the stomach and intestine, impeding the passage of food. This manifests as difficulty swallowing and vomiting. The problem is often resolved endoscopically by bougienage of the narrowed area.
- Dumping syndrome. This condition is associated with the rapid passage of undigested food from the reduced stomach into the small intestine. The body responds by releasing insulin and redistributing fluid, which causes weakness, sweating, palpitations, and diarrhea.
- Nutrient deficiency. Since the surgery limits absorption in the bypass segment,There is a lifelong risk of developing vitamin and mineral deficiencies, primarily B vitamins, D, iron, and calcium. This is not a complication in the strict sense, but a systemic consequence that requires ongoing compensation through specialized vitamin and mineral supplements.
It should be emphasized that with modern surgery and the use of high-tech equipment, the likelihood of developing serious complications is minimized.
Treatment, rehabilitation, prevention
Patient Stories
Anna, 36 years old.
"My weight problem began after the birth of my second child. Hormonal changes and stress led to my weight reaching 120 kg. I tried not to look in the mirror and avoided meeting people. My joints constantly ached, and the sidelong glances in public became unbearable. My attempts to lose weight ended in failure and the extra pounds returned.
After gastric bypass, everything changed. The weight loss process was gradual but steady. After just 10 months, I weighed 75 kg. And, most surprisingly, the constant craving for sweets disappeared, I had energy for walks with the children, and my usual clothes became hopelessly big."
Marina, 42 years old.
"My path to bypass surgery began with a diabetes diagnosis at 38. Weighing 117 kg, I was also taking hypertension medications, feeling my health deteriorate with each passing year. Constant fatigue, numbness in my legs, and fear of the future became my constant companions. Attempts to lose weight through diets ended in failure. At the K+31 clinic, I was offered a comprehensive solution—a comprehensive treatment program under the supervision of a bariatric team. I read numerous reviews and was mentally prepared. Preoperative preparation with an endocrinologist was especially important for me. We carefully adjusted my therapy to minimize risks. The surgery itself was performed laparoscopically, which allowed me to recover quickly. I was home on the third day. The most significant changes began in the first few months, and by the end of the first year, my weight had stabilized at 72 kg."
Prices for surgery

Patient questions
Can gastric bypass be reversed?
Gastric bypass is an irreversible procedure. Restoring the digestive tract to its original condition is associated with extremely high risks and technical complexity, and is therefore performed only in exceptional cases.
How painful is the surgery and recovery period?
The procedure is performed under general anesthesia, so there is no pain during the procedure. Moderate discomfort is possible in the postoperative period, but it is effectively relieved with modern analgesics. Thanks to the laparoscopic technique with minimal incisions, most patients report satisfactory well-being within 2-3 days after the procedure.
How long after surgery can I plan to become pregnant?
Experts recommend postponing pregnancy planning until weight stabilization, which usually occurs 12-18 months after surgery. This period allows the body to adapt to the new diet, stabilize hormonal levels, and replenish vitamin deficiencies. Pregnancy after bypass surgery requires special monitoring, but with proper guidelines, it usually proceeds smoothly.
What happens if you break the diet?
Deviating from the diet can lead to dumping syndrome, which is characterized by sudden weakness, sweating, increased heart rate, and abdominal discomfort. These sensations act as a natural limiting factor. Furthermore, systematically violating the diet reduces the effectiveness of the surgery and can lead to insufficient weight loss.

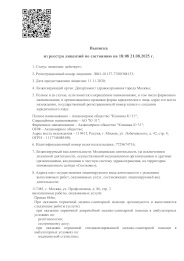
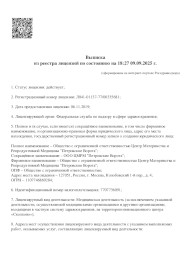
This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price


































































What is gastric bypass surgery?
Gastric bypass, or gastric bypass, is one of the most effective and sought-after areas of bariatric surgery—a field of medicine aimed at combating obesity and its consequences. This technique radically alters the anatomy of the digestive tract, leading to fundamental changes in the digestion process.
The surgery involves creating a new, significantly reduced stomach volume and reconstructing the food passages. A small reservoir, approximately 20-30 ml in volume, is surgically created from the upper, most active part of the stomach. This artificially created small stomach is almost immediately connected to the small intestine—not to its initial section, but to a section located some distance from the duodenum. As a result, food travels a shortened route—from the small stomach directly to the middle section of the small intestine. In this case, a significant portion of the main stomach, the duodenum, and the initial segment of the jejunum are excluded from the digestive process, although they continue to function, participating in the secretion of digestive juices.
The effectiveness of the bypass is explained by two mechanisms.
This dual mechanism of action, involving reduced food intake and reduced absorption, ensures sustainable weight loss and promotes metabolic normalization, particularly in remission of type 2 diabetes.