Colorectal Cancer
Colorectal cancer is a malignant tumor of the colon and rectum. It is often referred to when talking about bowel cancer. It is one of the most frequently diagnosed malignancies today.

specialists

equipment

treatment

Causes of colon cancer
When cells in the lining of the colon or rectum malfunction and begin dividing uncontrollably, a tumor forms, growing and disrupting tissue, organs, and bodily functions. Risk factors for colon cancer include age, heredity, benign polyps, chronic inflammation, excess weight, unhealthy habits, and poor diet. Smokers, heavy drinkers, the elderly, obese individuals, and those with family members diagnosed with colon cancer or familial adenomatous polyposis are more likely to suffer from this disease.
Two main factors can contribute to the development of cancer of the rectum or other parts of the colon: poor diet and a hereditary predisposition. The main dietary factors that cause colorectal cancer include the following:
- Lack of dietary fiber
- Excess or predominance of animal fats in the daily diet
- Overeating
- Alcohol abuse
Foods high in fiber and low in saturated and trans fats have an anti-cancer effect. Foods rich in vitamins D, C, and calcium reduce the risk of colon cancer.

Provoking factors
In addition to heredity and dietary factors, there are a number of factors that directly increase the risk of developing malignant intestinal tumors. Negative effects on the mucosa disrupt normal cell division, creating conditions conducive to cell degeneration. The main factors that trigger cancer include:
- Carcinogens – ingested through food, tobacco smoke, and alcohol – can damage intestinal wall cells.
- Chronic inflammation – with ulcerative colitis or Crohn's disease, tissues are constantly damaged and more susceptible to mutation.
- Infections – some viruses and bacteria cause structural changes in mucosal cells.
- Bad habits – smoking and regular alcohol consumption significantly increase the risk of cancer.
Numerous scientific studies confirm a genetic predisposition to colorectal cancer. Scientists particularly highlight the link between gene mutations and the development of polyposis and non-polyposis hereditary cancers. Changes are observed in the MLH1 and MSH2 genes, so if these abnormalities are detected, the entire family should undergo thorough diagnostic testing. Those at risk should undergo periodic colorectal cancer screening to detect malignant tumors at an early stage.

Other causes of colorectal cancer include:
- Polyps, adenomas, and other benign neoplasms of the colon
- Crohn's disease
- Chronic colitis
- Weakened immunity
- Exposure to carcinogens
- Chronic infections
- Human papillomavirus
- Tumors of the female genital area, breasts
- Chronic inflammatory bowel disease
The presence of several factors that affect the body over a long period of time is especially dangerous. Cancer often develops at the site of polyps, which can eventually become malignant.
Risk factors for colorectal cancer may also include age over 55 (63 for rectal cancer), a sedentary lifestyle, smoking, and alcoholism. Certain medical conditions, such as diabetes, acromegaly, or gallstones, also increase the risk of developing colorectal cancer.
All of the above-mentioned causes and risk factors can cause mutations in intestinal cells. And some of these mutations can lead to malignant tumors. A cellular condition in which the risk of mutations under the influence of certain factors is higher than normal is called microsatellite instability. This instability is the cause of colorectal cancer in 5% of cases and can lead to chromosome damage or DNA repair systems. Microsatellite instability in colorectal cancer occurs when the DNA of intestinal cells contains genes whose mutations lead to the development of tumors. A considerable body of scientific literature has been written on the mechanisms by which these mutations arise and the development of colorectal cancer, allowing for the development of effective treatment methods for each specific case.
Risk groups for developing bowel cancer
Color cancer can occur in anyone, but certain categories of patients are more likely to develop the disease:
- People over 55: With age, genetic damage (mutations) accumulates in the cells of the intestinal lining. Cellular DNA repair mechanisms become less effective, increasing the risk of malignant cell transformation.
- Patients with intestinal polyps.
- Persons with chronic inflammatory diseases of the gastrointestinal tract.
- Persons with a hereditary predisposition to cancer.
- Patients with diabetes: High insulin levels in the blood can stimulate tumor cell growth.
It is especially important for people at risk to pay close attention to their health and undergo regular examinations by an oncologist.
Types of colon cancer
Malignant colon tumors can be divided into the following types based on their growth patterns:
- Exophytic – tumors grow vertically, into the lumen of the colon
- Endophytic – tumors grow horizontally, within the wall of the colon
- Mixed tumors – combine both growth patterns
Benign colon tumors include tubular adenoma, tubulovillous adenoma, villous tumor, and adenomatous polyp of the colon. These tumors also pose a risk and require regular patient examinations, as colon cancer can develop from these benign tumors.
Based on histological characteristics (the type of cells from which the tumor originates), colon cancer is divided into the following types: adenocarcinoma, squamous cell carcinoma, solid tumor, melanoma, high-density carcinoma (scirrhous carcinoma), and signet-ring cell carcinoma of the colon. Adenocarcinoma, which develops in the cells of the inner lining of the colon or rectum, is the most common type.
Based on the degree of cell differentiation (i.e., how similar the tumor cells are to those from which they developed), colon cancer can be divided into:
- Well-differentiated tumors – malignant tumor cells are very similar to the healthy cells from which they developed.
- Moderately differentiated
- Poorly differentiated
- Undifferentiated – tumor cells are very different from healthy colon cells.
Metachronous cancer is a multiple cancer in which two or more primary tumors develop. Metachronous sigmoid colon cancer is the most common type. Metachronous rectal cancer is the second most common type.
Signs of colorectal cancer
As often happens with cancer, colon cancer can develop gradually, and the malignant tumor may remain undetected for a long time. This is precisely the time period when early diagnosis of colon cancer helps initiate effective, appropriate treatment, leading to a full recovery. Unfortunately, colorectal cancer often makes its presence known at stages when the tumor has already invaded the intestinal wall and metastasized. Therefore, it is important to pay attention to even minor signs of colorectal cancer.
In the early stages, colon cancer is asymptomatic, but as the malignant tumor grows, pain, increased gas, a feeling of heaviness, bloating, and irregular bowel movements begin to appear.
Worrying symptoms that require immediate medical attention include the following:
- Blood in the stool
- Changes in bowel habits, frequent constipation, diarrhea
- Mucus discharge from the anus
- Pain in the abdomen and anus
- Unexpected weight loss
- The appearance of symptoms associated with anemia, such as pale skin, shortness of breath, increased heart rate, lethargy, and drowsiness
- Weakness during the day
- Painful urge to defecate./li>
Similar symptoms also appear with metachronous colon cancer, especially weakness, pain, and bloody discharge and/or mucus. In sigmoid colon cancer, mucus and blood coat the stool, while in cecum cancer, they mix with the stool. In colon cancer, tarry stools appear.
Local and non-specific symptoms
In its early stages, colon cancer can present without obvious symptoms, so it's important to know the signs that may indicate the disease's progression. Symptoms are generally divided into two groups: local and nonspecific.
Local symptoms include changes directly related to bowel function: blood or mucus in the stool, abdominal pain or heaviness, and bowel disturbances such as constipation or diarrhea. These signs appear as the tumor grows and affects the intestinal mucosa and patency.
Nonspecific symptoms reflect the general condition of the body and do not always immediately indicate intestinal damage. These include weakness, fatigue, unexplained weight loss, and the development of anemia. These symptoms often accompany various diseases, but when combined with local symptoms, they can be an important signal to consult a doctor.
Symptoms of anemia are associated with cancer of the ascending colon. Tumors in this area can disrupt the body's hematopoietic functions.
It is important to pay close attention to the appearance of any of the described symptoms of colorectal cancer, which should be discussed with your doctor during your consultation. A qualified and experienced doctor will carefully inquire about the presence of any dangerous symptoms during the interview, which will help identify key signs of colon cancer.
Constipation and diarrhea, pain, blood in the stool, as well as false urges, nausea and vomiting, and fluid in the abdomen are all symptoms of colon cancer in its late stages.
The symptoms of colorectal cancer in men and women are the same. In addition to those described above, patients with colorectal cancer may also suffer from headaches, decreased performance, loss of appetite, and other symptoms. Unfortunately, malignant tumors in the colon can develop for more than ten years without causing any symptoms.
At an early stage, in the absence of a clear clinical picture, the only way to rule out the risk or detect colorectal cancer today is through preventive colonoscopy. This is recommended after age 45-50, especially for those at risk.
Stages of colorectal cancer
The TNM staging system for colon cancer determines the extent of tumor spread and the presence of metastases in nearby lymph nodes and other parts of the body: T is the extent of the primary malignant tumor's spread: T1 - the tumor has invaded the intestinal mucosa, T2 - it has spread to the muscular layer, T3 - all layers of the intestine have been affected, T4 - the malignant tumor has invaded adjacent tissues and organs. N is the number of regional lymph nodes affected: N0 - the tumor has not invaded the lymph nodes, N1 - metastases are present in 1-3 lymph nodes, N2 - in four or more lymph nodes; M is the presence of distant metastases: M0 - none, M1 - distant metastases are present.
The extent of tumor development is determined by its spread relative to the intestinal wall. This determines the severity of the clinical picture and the prognosis for treatment.

It is customary to distinguish 4 stages of colorectal cancer:
-
Stage I colon cancer
The tumor is confined to the intestinal wall. The patient has no complaints; mucus may be released during bowel movements. The cancer cells have not spread to the regional lymph nodes, and there are no metastases. With timely treatment, the prognosis for recovery is favorable.
-
Stage II colorectal cancer
The lesion spreads throughout the colon walls, possibly invading adjacent tissue. No metastases are detected. Symptoms of colon cancer include rectal discomfort, comparable to the presence of a foreign body. Discomfort in the lower abdomen may also occur, and blood may be present in the stool along with mucus.
-
Stage III colon cancer
Due to the tumor's growth, rectal patency is impaired. This stage may occur with or without metastases to the regional lymph nodes surrounding the rectum. The tumor invades surrounding tissue, tissue, adjacent organs, and more distant lymph nodes. The patient's condition worsens, and symptoms such as bloating, abdominal rumbling, and a false urge to defecate are added to existing symptoms. Complaints include pain, cramping, blood in the stool, diarrhea, and constipation. As colon cancer progresses, general weakness increases, performance and appetite decrease, and pallor develops.
-
Stage IV colon cancer
Terminal stage IV colorectal cancer, in which the malignant tumor reaches its maximum extent. The risk of bowel dysfunction and damage to adjacent organs increases. Metastases spread to distant lymph nodes, lungs, liver, bones, and stomach. Severe clinical manifestations of colon cancer include intestinal obstruction, vomiting, constipation, and gas retention. The patient complains of abdominal pain, which radiates to the organs affected by cancer cells. Severe exhaustion and signs of central nervous system damage are observed.
Modern methods of treating cancer of the rectum and other parts of the colon
Colon and rectal cancer are treated by oncologists, surgeons, colorectal surgeons, as well as chemotherapists, radiation therapists, and gastroenterologists. Currently, colorectal cancer is treated with surgery, radiation, and chemotherapy. Innovative approaches include the use of immune-based and biologic agents. The choice of treatment for colon cancer depends on the type of cancer, its stage, tumor location, age, and the presence of comorbidities.
Radiation therapy for colon cancer
It is chosen by the treating physician when, prior to surgery, it is determined that the entire intestinal wall is involved, and metastases are detected in the lymph nodes. Radiotherapy is an effective method of treating malignant tumors during the preoperative stage. Radiation therapy is often used to treat rectal cancer due to its tendency to recur. It is administered before and/or after surgery. It can cause side effects such as intestinal obstruction or rectal bleeding.
Chemotherapy for colon cancer
For colorectal cancer, chemotherapy is used as adjuvant therapy before surgery to shrink the tumor or after surgery to destroy remaining cancer cells. In advanced stages, chemotherapy is used as a palliative treatment, aimed at relieving symptoms and prolonging the patient's life. Capecitabine, irinotecan, oxaliplatin, and some other chemotherapy drugs are used to treat colon cancer, usually in combination.
Combination of radiation therapy and chemotherapy
It is used for local tumor cell spread, regional lymph node involvement, and intestinal fascial invasion with tumor immobility relative to the pelvis. It is used to treat rectal cancer and other parts of the colon.
Preliminary clinical, histological, and instrumental examinations allow for the proper development of a treatment program. A comprehensive approach ensures support during radiation therapy and chemotherapy, as well as high-quality care in the postoperative period.
Surgical intervention
The most effective treatment for colorectal cancer is surgical removal of the malignant tumor. This often includes removal of part of the colon or rectum and nearby lymph nodes.
If the tumor is large enough and its growth is confined to the mucosa and submucosa, modern surgery is performed endoscopically.
Transanal endoscopic microsurgery. Ensures maximum preservation of the intestinal wall and a comfortable postoperative recovery period.
Open or laparoscopic surgery. This is chosen when the tumor has reached the muscular layer. The entire section of intestine involved is removed. Adjacent lymph nodes and fat are also removed. Laparoscopic surgery is prescribed for the treatment of cancer of the cecum, certain sections of the colon, and rectum.
Colostomy for rectal cancer. In many situations, the location of the malignant tumor makes it impossible to preserve the anus, so a colostomy is performed. Temporary (remains until the rectum heals) and permanent (modern treatments for rectal cancer allow most patients to avoid it). Today's surgery is focused on maximizing organ function, which can be achieved by performing a prophylactic colostomy, which reduces the risk of infectious and inflammatory complications in the suture area. The colostomy is closed several months after surgery if the prognosis is favorable. Combined techniques are used by surgeons when multiple organs are involved in the tumor process. Distant metastases are removed sequentially.
Our clinic uses the most effective and safest methods for treating colorectal cancer, which are individually selected based on the individual patient's condition and tumor characteristics. After diagnosis, treatment for colorectal cancer begins as soon as possible.
Endoscopic stenting
Endoscopic stenting is used to treat intestinal obstruction, which often occurs in the late stages of colorectal cancer. Using an endoscope, the doctor inserts a metal stent into the narrowed section of the intestine. This method reduces pain, eliminates the risk of intestinal rupture, and allows the patient to more quickly return to a normal diet. Stenting is most often used as a palliative treatment when radical surgery is not possible. In other cases, the procedure helps stabilize the patient's condition and prepare them for elective surgery or chemotherapy.
Targeted therapy for colorectal cancer
The study of cancer cells has revealed their molecular characteristics and differences from normal cells. This has led to the development of drugs that target tumor cells and spare healthy tissue. Targeted therapy for colorectal cancer uses substances that identify specific tumor cell receptors, blocking their ability to stimulate their own growth or the growth of blood vessels that supply nutrients and oxygen to the tumor. Today, targeted therapy is used to treat colorectal cancer in its late stages.
Immunotherapy for colon cancer
This is a relatively new treatment method that aims to activate the body's own immune system to fight cancer cells. Drugs such as nivolumab and pembrolizumab are used to treat colon cancer.
Rehabilitation after treatment
Rehabilitation after colorectal cancer treatment is a complex process aimed at fully restoring the patient's physical and psychological well-being, as well as minimizing the risk of recurrence.
Key points for successful rehabilitation:
- Nutrition: The patient is prescribed a gentle, balanced diet. It is important to avoid foods that cause flatulence, constipation, or intestinal irritation. To normalize bowel movements, it is necessary to maintain a hydration regimen. Physical activity: Returning to physical activity should be gradual and consistent. This can begin with daily leisurely walks in the fresh air, breathing exercises, and light exercises aimed at gently strengthening the abdominal and pelvic floor muscles. Psychological support: A difficult diagnosis and long-term treatment can be a difficult emotional ordeal for many patients. An experienced psychologist or psychotherapist specializing in working with cancer patients will help overcome fears of relapse and anxiety, and teach stress management and relaxation techniques.
- Regular checkups: a mandatory part of rehabilitation, aimed at the early detection of possible cancer complications or side effects of therapy.
Prevention of Rectal and Colon Cancer. Prognosis
Even with the most modern treatments for colorectal cancer, the possibility of remaining cancer cells in the body cannot be ruled out. Their size is so microscopic that effective diagnosis becomes impossible. However, cancer cells can cause recurrence. The likelihood of recurrence is higher the sooner a recurrence is detected. To prevent recurrence, after surgery, chemotherapy, and hospital discharge, patients are advised to regularly visit their doctor and undergo the recommended diagnostic procedures. Even after successful treatment, there is a risk of polyps, which can eventually develop into malignant tumors.
The first two years after completion of treatment are a period of increased risk of recurrence, so examinations during this time should be especially thorough. During this period, visits to the doctor should be every three months, and every six months during the following three to five years. During the consultation, the doctor will conduct an examination, prescribe tests for tumor markers, and refer you for an X-ray, colonoscopy, ultrasound, and CT scan. The risk of cancer recurrence decreases five years after surgery.
Preventive measures that reduce the risk of colorectal cancer include:
- Preventive colonoscopy. Helps identify chronic inflammatory processes and polyps.
- A balanced diet, including foods high in fiber.
- Avoid exposure to carcinogens.
- Strengthen the body's immune system, preventing its weakening.
- Manage stress.
- Active lifestyle.
- Normalize sleep.
- Prevent infection with the human papillomavirus.
The five-year survival rate for patients with colon cancer after treatment is 90-95% at stage I, 65-90% at stage II, 50-70% at stage III, and approximately 11% at stage IV.
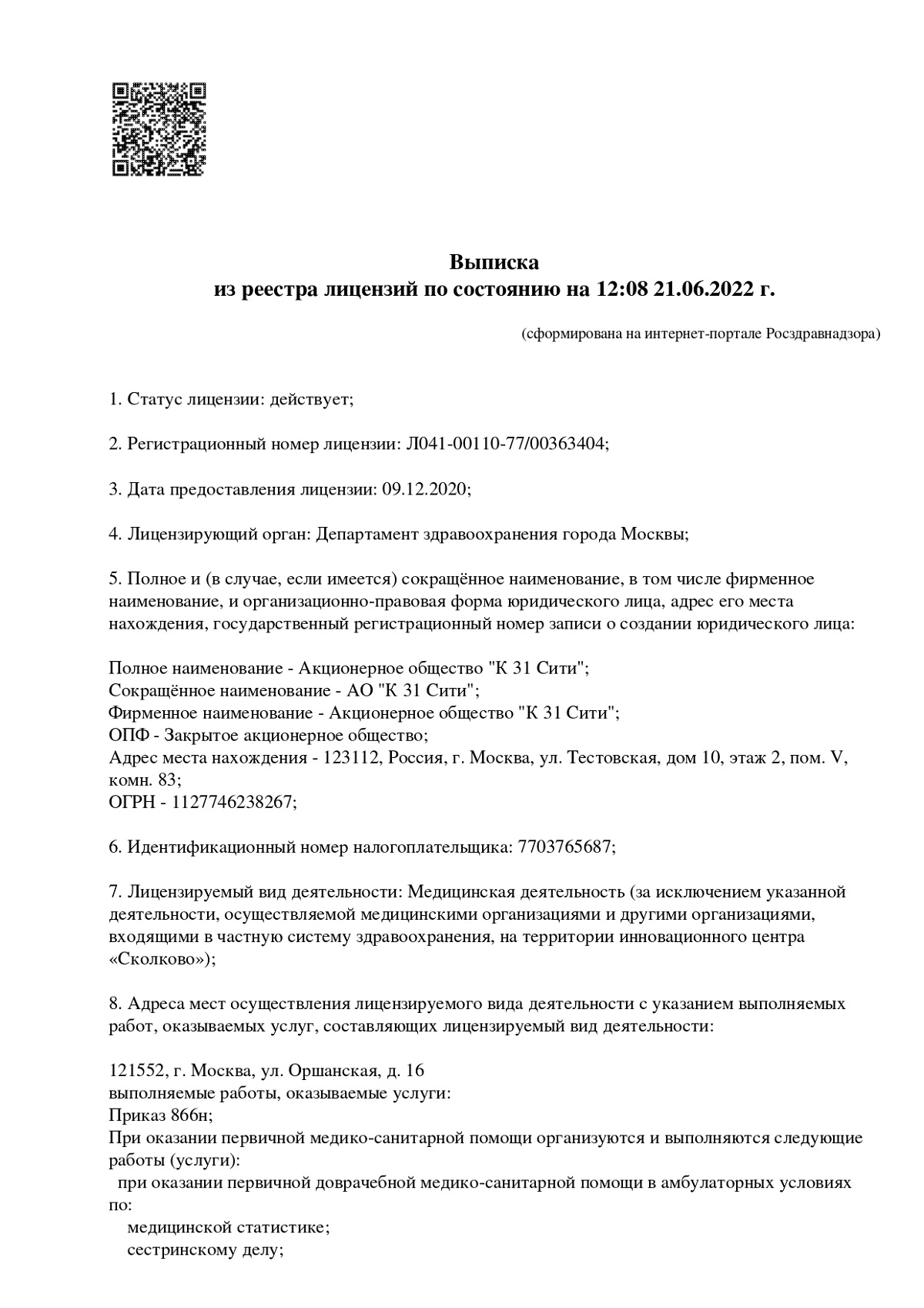
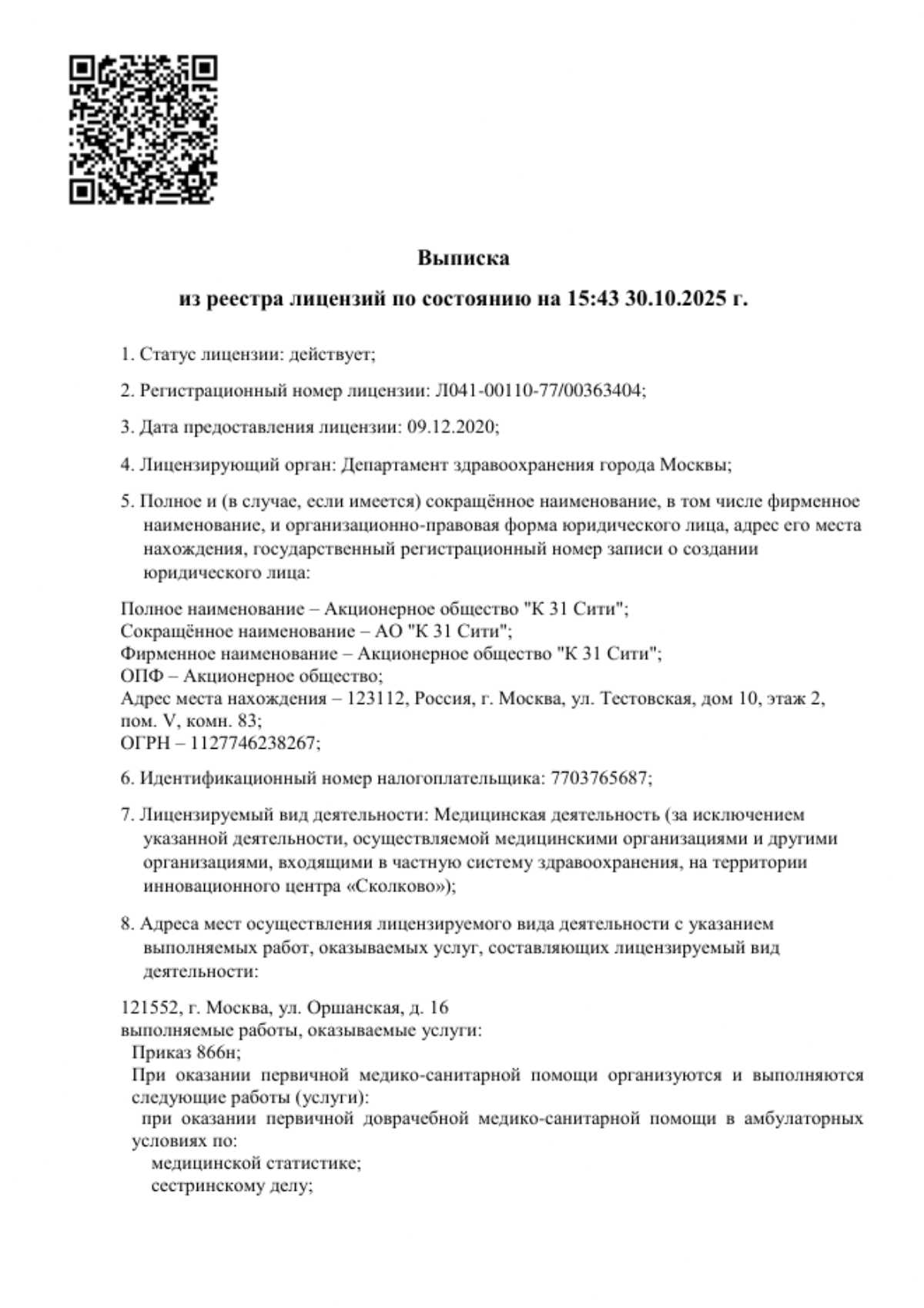
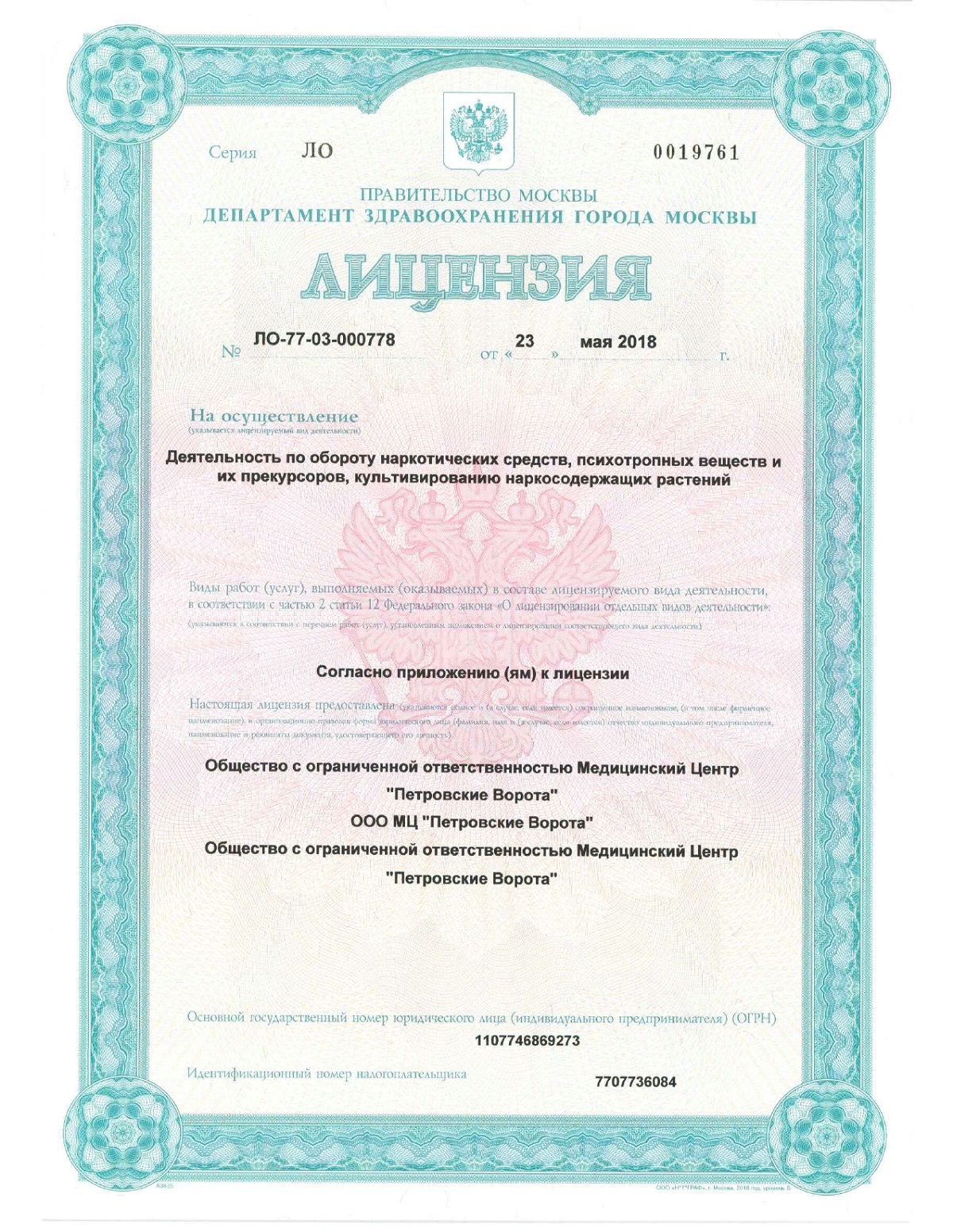
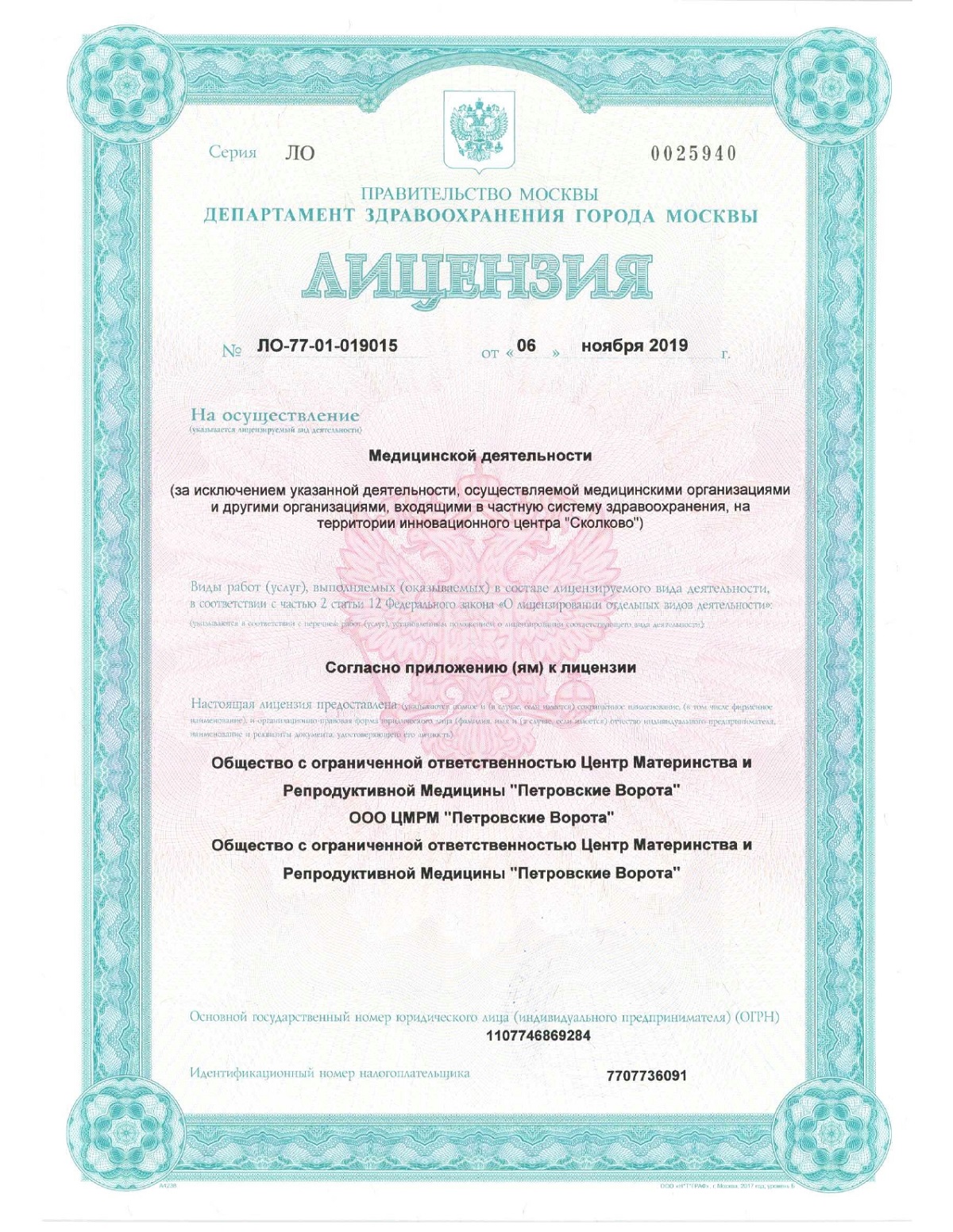
Our clinic's oncology department is equipped with modern equipment for diagnostics, instrumental examination, and laboratory testing of the intestines. Our doctors use only the most effective and safe treatment methods. If cancer is diagnosed, patients will be provided with all the latest information and access to our clinic's full range of treatment options. Our inpatient department offers comfortable conditions and a welcoming environment for physical and emotional well-being.
Our K+31 centers treat breast cancer, stomach cancer, kidney cancer, and other oncological diseases. Call us or schedule an appointment online.
Frequently Asked Questions
We provide answers to our patients' most pressing questions.
How do you know if you have colon cancer?
Colorectal cancer often develops without obvious symptoms. In its early stages, the disease may manifest itself as blood in the stool, abdominal pain or cramps, sudden weight loss, and changes in bowel habits. These symptoms do not always indicate the development of cancer, but if they appear, it is important to consult a doctor. A diagnosis is made only after a comprehensive examination.
How long can you live with colon cancer?
When cancer is detected at stage I, the chance of surviving more than five years reaches 90%. In later stages, the prognosis is worse, but modern treatment methods and supportive care allow for maintaining quality of life for as long as possible.
How quickly does colon cancer progress?
Colorectal cancer develops slowly in most cases. It can take several years from the appearance of the first cells to a full-blown tumor. This is why doctors recommend regular screening after age 45 to detect the disease at an early, asymptomatic stage. Early diagnosis makes it possible to halt the progression of the disease and facilitate treatment.
Colon cancer treatment costs
Colorectal cancer treatment prices in Moscow depend on the treatment method, stage of the disease, and duration. In the early stages, surgery may be sufficient and less expensive than a comprehensive program. At later stages, chemotherapy, radiation therapy, or targeted drugs are used, so the cost increases significantly.
The cost of colorectal cancer treatment includes diagnosis, the procedure itself, and medical follow-up. Each treatment plan is developed individually, so the exact cost can only be determined after an in-person consultation with a specialist.
What do we treat
Price
Make an appointment at a convenient time on the nearest date
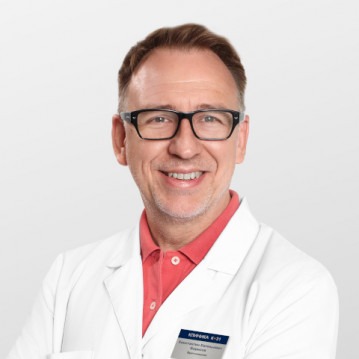
Our doctors

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Other cancer treatment services






























































Definition and types of colorectal cancer
Colorectal cancer is a malignant neoplasm characterized by the uncontrolled growth of atypical cells. Tumors can develop in both the colon and small intestine. One of the most common types of the disease is colorectal cancer. Small intestinal cancer is less common but still poses a serious health threat.
It is important to understand the difference between benign and malignant intestinal tumors. Benign tumors, such as adenomas or polyps, grow slowly, do not metastasize, and are not life-threatening if removed promptly. Malignant tumors tend to grow aggressively, destroy the intestinal wall, and spread to other organs. Therefore, early diagnosis is essential for a successful, uneventful recovery.
As the pathological process progresses, the lesion spreads into the intestinal lumen, or the tumor invades surrounding tissue. The disease can metastasize, so early diagnosis is especially important, as it increases the chances of effective treatment. The risk of colorectal cancer increases after age 45, peaking at 70–75 years, and is more prevalent in men.
The intestine, an organ whose main function is digestion, is divided into two sections: the small intestine and the large intestine. This article focuses on colon cancer.
The human large intestine, in turn, consists of six sections: the cecum, the four colons (ascending, transverse, descending, and sigmoid colon), and the rectum. Malignant tumors can develop in any of these sections, but cancer most commonly occurs in the rectum, the final section of the intestine where feces are stored and eliminated.