Treatment of Brain Oncology (Tumor, Cancer)
A diagnosis of brain tumor requires detailed consideration and a clear action plan. The main feature of the disease is its anatomical location. The brain is a structure confined to the limited space of the skull, where any tumor inevitably leads to compression of the surrounding tissues and impairment of their function.
At the K+31 Clinic in Moscow, patients with central nervous system oncology are treated using a multidisciplinary consultation. The decision on treatment strategy is made jointly by a team of neurosurgeons, oncologists, chemotherapists, and radiologists. This approach allows us to develop a personalized and most effective strategy for each patient.

specialists

equipment

treatment
Benign tumors
The term "benign" describes the biological properties of the tumor, but does not negate its clinical significance. Characteristics of such a neoplasm:
- It has a slow growth rate
- It has clear boundaries. The tumor does not invade the brain, but pushes it away as it grows.
- Its cells are highly differentiated, meaning their structure is close to normal.
The clinical manifestations (main symptoms) of such a neoplasm are caused by the mass effect – pressure on functionally important areas of the brain. If the tumor is resectable, that is, accessible to a surgeon, the primary treatment method is total surgical removal. In many cases, this leads to a complete cure.

Malignant tumors
This group of tumors is what is more accurately called brain cancer. Their biological behavior is fundamentally different:
- Rapid, infiltrative growth. This means that the tumor invades healthy brain tissue without clear boundaries. Imagine a drop of ink falling on a blotter.
- Significant cellular atypia (cells are very different from normal)
- High potential for recurrence – regrowth after treatment.
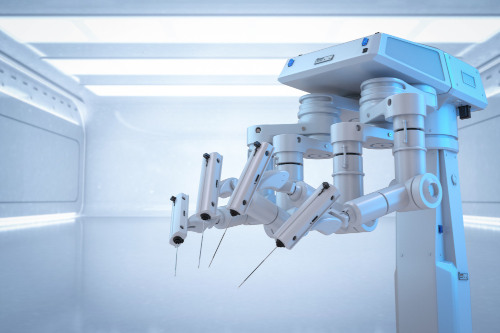
Malignant tumors require combination therapy. Treatment typically includes several methods: neurosurgery to safely remove as much of the visible tumor as possible, followed by radiation therapy and/or chemotherapy to target any remaining cancer cells. Accurate diagnosis and staging are crucial in planning all subsequent steps.
Causes and risk factors
The question every patient asks: Why did this happen to me? What is the cause? It must be acknowledged: in the vast majority of cases, a single, precise cause for a primary brain tumor cannot be determined. This is not a disease that can be directly linked to lifestyle or bad habits. The tumor's development is the result of a spontaneous genetic mutation in one of the cells. A random glitch.
However, medicine has identified a number of factors that can increase the risk of developing such tumors. It is important to understand that these are statistical correlations, not direct causes.
- Ionizing radiation. High doses of radiation, especially those received in childhood (for example, during radiation therapy for another condition), have been shown to increase the risk of developing head tumors later in life. This is the most significant known risk factor.
- Hereditary genetic syndromes. There are a number of rare inherited diseases, such as neurofibromatosis, Li-Fraumeni syndrome, and tuberous sclerosis. They significantly increase the risk of developing CNS tumors. However, they account for only a small percentage of all cases.
- Age. The risk of developing most brain tumors increases with age. The peak incidence occurs in older people. However, some types of tumors (for example, medulloblastoma) are specific to childhood.
- Immune deficiency. Patients with congenital or acquired immunodeficiency (for example, after organ transplantation or HIV infection) have a higher risk of developing certain tumors, particularly CNS lymphomas.
Cell phones, power lines, and head injuries—to date, there is no convincing scientific evidence confirming a link between these and brain cancer.
Symptoms of brain tumors
General symptoms
These symptoms are a consequence of increased intracranial pressure. The growing tumor occupies a confined space within the skull, compressing the brain and disrupting the circulation of cerebrospinal fluid.
- Headache. This is the most common symptom. But this is not a typical headache. The tumor is characterized by a dull, aching pain, often occurring in the morning and intensifying with coughing, sneezing, and straining. It is poorly relieved by conventional analgesics.
- Nausea and vomiting. The classic symptom is vomiting at the peak of the headache, which does not bring relief. This is not caused by stomach problems, but by direct irritation of the vomiting center in the brain.
- Dizziness and loss of balance. A feeling of unsteadiness and unsteadiness when walking.
- Seizures. The sudden onset of an epileptic seizure in an adult who has never had one is a very alarming symptom that requires immediate diagnosis. [The text appears to be incomplete and likely a mistranslation.]
- Disturbances in consciousness and mental state. Drowsiness, lethargy, behavioral changes, decreased memory and concentration. The patient becomes apathetic and indifferent.
Focal symptoms
These symptoms directly indicate which part of the brain is affected. They arise due to the destruction or compression of a specific functional center by the tumor.
- Movement disturbances. Weakness in an arm or leg (paresis), up to complete paralysis.
- Sensory disturbances. Numbness, tingling, a "pins and needles" sensation in the limbs or face.
- Speech disturbances. The patient has difficulty finding words, their speech becomes slurred (motor aphasia). Or they stop understanding speech addressed to them (sensory aphasia).
- Visual disturbances. Visual field loss (the person cannot see part of the space), double vision, decreased visual acuity.
- Coordination disturbances. Failure to perform precise movements, clumsiness, and unsteadiness of gait (ataxia). This symptom often indicates a problem in the cerebellum.
- Auditory and olfactory hallucinations. The appearance of extraneous sounds or odors that are not actually present.
- Hormonal imbalances. This symptom is characteristic of tumors of the pituitary gland and hypothalamus.
The appearance of any of these symptoms, especially if they develop gradually and steadily progress, is an absolute indication for immediate medical attention and a comprehensive diagnosis.
Brain Cancer Stages
A common question from patients: what stage is my cancer? This requires clarification. The classic TNM (Tumor, Nodus, Metastasis) staging system, which is used to stage most cancers (for example, lung or colon), is rarely used for primary brain tumors. Why is this?
Firstly, primary brain cancer very rarely metastasizes beyond the central nervous system. Its aggressiveness manifests itself in local, infiltrative growth, destroying the tissue around it.
Secondly, even the smallest benign tumor, located, for example, in the brainstem, can be fatal. A large tumor in the frontal lobe, however, can remain asymptomatic for a long time. Size does not always determine the prognosis.
Therefore, neuro-oncology uses a different system—the Grade classification developed by the World Health Organization (WHO). It is based on the histological structure of the tumor, that is, how its cells appear under a microscope.
- Grade I. These are benign tumors. The cells are almost normal and grow very slowly. With complete removal, the prognosis is excellent.
- Grade II. The tumor is still considered conditionally benign or low-grade malignancy. The cells begin to deviate from the norm, growth is slow, but there is a tendency for infiltration and recurrence. Over time, such a tumor can progress to a higher grade of malignancy.
- Grade III. This is clearly a malignant process. The cells are atypical, dividing actively. The tumor infiltrates the brain. The prognosis is grave.
- Grade IV. The most aggressive stage. The cells are extremely atypical, growing very rapidly, and the tumor contains foci of necrosis (tissue death). An example is glioblastoma.
Determining the degree of malignancy (grade) is the primary diagnostic task. It is this grade, not the conventional "stage," that determines the choice of treatment strategy.
Diagnosis of brain tumors
Making an accurate diagnosis of a suspected brain tumor is a complex process. It requires the use of high-tech imaging techniques and, ultimately, obtaining a tissue sample for examination. A diagnosis of brain cancer cannot be made based on symptoms alone.
Diagnostic Methods
The foundation of modern brain tumor diagnostics is neuroimaging.
- Magnetic resonance imaging (MRI). This is the "gold standard." MRI allows us to visualize the brain itself, its structures, membranes, and, ultimately, the tumor itself with exceptional accuracy. We can see its precise location, size, and relationship to important functional areas.
- MRI with contrast. For better tumor visualization, a special gadolinium-based contrast agent is injected into a vein. Malignant tumors typically have a well-developed vascular network and actively accumulate contrast, becoming bright and "glowing" on the images. This helps distinguish them from benign tumors and other processes (for example, the consequences of a stroke).
- Computed tomography (CT). CT better visualizes the bony structures of the skull. This method is often used in emergency situations to quickly rule out hemorrhage. For a detailed diagnosis of the tumor itself, CT is less informative than MRI.
- Positron emission tomography (PET-CT). This is a functional imaging technique. The patient is injected with radioactive glucose. Cancer cells actively consume it, causing the tumor foci to glow on the images. PET-CT helps assess the degree of tumor malignancy and distinguish relapse from postoperative changes.
Examination and confirmation
MRI results provide a preliminary diagnosis. We can determine with a high degree of certainty the tumor type. But a definitive, 100% diagnosis can only be made one way: by obtaining a sample of tumor tissue and examining it under a microscope. This is called histological verification.
How can this be obtained?
- Biopsy. If the tumor is located in a difficult-to-reach or functionally significant location, a stereotactic biopsy is performed. Using a special navigation system, the surgeon inserts a thin needle precisely into the tumor through a tiny opening in the skull and takes a small tissue sample.
- During tumor removal surgery. If immediate surgery is planned, the tissue sample taken during surgery is sent for histological examination. Sometimes, a rapid analysis is performed during surgery so the surgeon can adjust the extent of the removal.
After examining the tissue, the pathologist makes a final diagnosis: the exact type of tumor and its grade. Only then can the correct and most effective treatment strategy be developed.
When to see a doctor
A brain tumor isn't a condition you can easily miss if you're paying attention. You should immediately consult a neurologist or primary care physician if you experience the following symptoms, especially if they appear out of the blue and worsen over time:
- Unexplained, persistent headache, especially in the morning
- First-ever epileptic seizure
- Weakness or numbness in an arm or leg
- Speech, vision, or coordination problems
- Sudden changes in behavior, memory, or thinking
Timely diagnosis is the key to successful treatment.

Frequently Asked Questions
Can brain cancer be cured?
Some types of tumors, especially benign ones, can be completely cured with surgical removal. For malignant tumors, the goal of treatment is to achieve long-term remission and maximize quality of life.
Is brain surgery painful?
Brain tissue itself has no pain receptors. The surgery is performed under general anesthesia, making it completely painless. Postoperative pain in the incision area is usually moderate and well controlled with medication.
Does hair loss occur during brain tumor treatment?
Hair loss can occur in the treated area during radiation therapy. During chemotherapy, hair loss depends on the specific drug, but brain tumor treatments often use regimens that do not cause total alopecia.
Bibliography
- The textbook "Oncology" edited by V.I. Chissov and S.L. Daryalova, published by GEOTAR-Media in 2007.
- Neurology. National Guidelines. Brief Edition / edited by E.I. Gusev, A.N. Konovalov, A.B. Gekht. - Moscow: GEOTAR-Media, 2018. - 688 p. - ISBN 978-5-9704-4405-4.
- Sashin, D.V. Dissertation: Diagnostic Methods and Characteristics of Brain Tumors / D.V. Sashin. — Moscow: NMIC Oncology, 2020.
- Personalized Treatment of Brain Gliomas: Targeted Therapy, Patient-Specific Tumor Models (Review) / K.S. Yashin, D.V. Yuzhakova, D.A. Sachkova, L.S. Kukhnina, T.M. Kharitonova, A.S. Zolotova, I.A. Medyanik, M.V. Shirmanova – Article // Standards and Technologies of Medicine. – 2023. – No. 3.
Our doctors

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
News
What do we treat
Price










































































Definition and types of brain tumors
Any neoplasm is based on a pathological process in which a cell loses the ability to control its own division. As a result, a nodule of abnormal tissue—a neoplasm—forms.
The primary classification divides all intracranial pathological growths into two categories.
The next step, which determines the treatment plan and prognosis, is histological verification of the tumor. It is necessary to determine whether it is benign or malignant.