Cervical Cancer: Diagnosis and Treatment
Cervical cancer is a malignant tumor that develops in the area where the cervix meets the cervical canal, a narrow area adjacent to the vagina. The disease can be asymptomatic for a long time, and its early signs, such as bleeding and discomfort, often go unnoticed. The main cause of this pathology is a persistent infection caused by oncogenic types of the human papillomavirus. Timely consultation with a gynecologist ensures a high chance of a full recovery.
Modern medicine allows not only to successfully treat this disease in its early stages but also to effectively prevent it through screening and vaccination. Comprehensive diagnostics and personalized cancer treatment, including surgical, radiation, and drug treatments, are provided at the K+31 Clinic in Moscow using cutting-edge equipment and internationally recognized specialists.

specialists

equipment

treatment
Classification and stages of cervical cancer

A classification system that takes into account the histological structure of the tumor and its extent in the body is used to determine patient management and prognosis.
Based on cellular structure, there are two main types of malignant cervical lesions:
- Squamous cell carcinoma. It develops from the flat epithelial cells lining the vaginal portion of the cervix – the ectocervix. This type is the most common, accounting for up to 80-90% of all diagnosed cases.
- Carcinoma. It develops from the mucus-producing glandular cells located in the cervical canal, affecting the endocervix. Cervical carcinoma is less common, but its incidence has been increasing in recent decades. This type also includes rarer forms: clear cell, mucinous, and others.
The stage of the pathology is determined according to the international FIGO classification based on the results of physical, instrumental, and morphological examinations. It reflects the anatomical distribution of the neoplasia.

- Stage 0 – preinvasive. Cancer cells are found only in the superficial layer of the epithelium, without invading the underlying tissue. This stage is also known as high-grade cervical intraepithelial neoplasia.
- Stage I. The tumor is limited to the cervix. Two substages are possible: IA: Microscopic invasion, detectable only histologically; IB: Clinically visible lesion, confined to the cervix.
- Stage II. The tumor extends beyond the uterus, involving the upper vagina or parametria, but does not reach the pelvic walls.
- Stage III. The pathological process affects the lower third of the vagina, the pelvic area, or leads to renal dysfunction.
- Stage IV. Characterized by the most extensive spread. There are two possible substages: IVA: Invasion of the mucosa of adjacent organs; IBB: Presence of distant metastatic lesions in the lungs, liver, bone tissue, and other organs.
Determining the FIGO staging system is necessary for choosing the optimal treatment plan, which may include both organ-preserving interventions in the early stages and radical surgery combined with combination therapy for advanced forms of the disease.
Diagnostic methods
Screening and laboratory testing
Today, programs aimed at detecting the disease in apparently healthy women before any symptoms appear are actively used. Their fundamental goal is to detect precancerous changes and early, clinically asymptomatic forms of cancer, when treatment is most effective and the prognosis is favorable.
Two methods are used:
- Cytology test (Pap test). During the analysis, cells collected from the surface of the cervix and cervical canal are examined under a microscope. A specialist evaluates their size, shape, and nuclear structure, identifying atypical elements.
- HPV testing. Polymerase chain reaction (PCR) can identify the presence of oncogenic types of human papillomavirus (HPV) in the body, even at minimal concentrations. [The phrase "PAP" appears to be a mistranslation.]
The optimal strategy is to combine Pap and HPV testing, which significantly increases screening sensitivity and allows for the determination of further patient monitoring strategies.
Examination and Biopsy
If suspicious symptoms are present or the initial screening results are positive, the diagnosis moves into a more in-depth phase. The specialist performs a visual and manual assessment of the reproductive tract:
- The texture and color of the cervical mucosa, as well as the presence of visible ulcers, growths, or areas of structural alteration, are assessed using a speculum.
- A bimanual examination determines the size, shape, and mobility of the uterus, and identifies possible parametrial tissue compaction or tenderness.
If abnormalities are detected, the doctor prescribes a more extensive instrumental examination. A colposcopy is performed. This is a detailed examination of the cervix under significant optical magnification. The mucosa is treated with acetic acid and Lugol's solution. Healthy and abnormal tissues react to the reagents differently: atypical areas do not stain, but remain light. This indicates the need for a targeted biopsy with histological examination to verify the diagnosis.
Removing a small tissue sample from the most suspicious area allows the doctor to examine not only individual cells but also the tissue structure as a whole. Histological analysis provides a definitive answer regarding the presence or absence of invasive cancer, its type, and degree of differentiation.
Predisposing factors and underlying causes
The underlying cause of this pathology is HPV infection. Strains classified as highly oncogenic produce the oncoproteins E6 and E7. These proteins inactivate cellular defense mechanisms by suppressing the functions of the tumor suppressors p53 and pRb, ultimately leading to genomic instability, uncontrolled proliferation, and malignancy of epithelial cells. Although types 16 and 18 bear the primary pathogenic burden, other strains, such as 31, 33, and 45, are also responsible for some cases.
HPV infection is an important, but not the only, condition for the development of this pathology. Even the presence of the virus in combination with additional risk factors does not automatically lead to cancer. The vast majority of cases of infection are resolved by the body's own immune system. But even if the virus is detected, it's important not to panic and instead focus on regular monitoring by a specialist and lifestyle changes. This approach can significantly reduce potential risks.

The risk of developing pathology increases significantly with the combined influence of the following factors:
- Tobacco smoking Carcinogenic resins have an affinity for the cervical epithelium. Traces of them are found in cervical mucus. They can enhance the negative effects of the virus, causing irreversible damage to cellular DNA and suppressing the local immune response, creating favorable conditions for the pathogen's proliferation
- Long-term hormonal contraception Taking combined oral contraceptives for five or more years without medical supervision is associated with an increased risk of malignancy. It is believed that steroid hormones can modulate the expression of viral oncogenes and promote neoplastic transformation of infected cells
- Early and active sexual activity with multiple partners These behavioral factors statistically increase the likelihood of infection with highly oncogenic HPV strains, creating a cumulative effect on the viral load and shortening the latency period for the development of precancerous lesions
- Chronic immunosuppression Decreased immune reactivity observed in HIV infection, after organ transplantation, or while taking immunosuppressants disrupts natural control over viral activity, accelerating the transition from dysplasia to invasive neoplasm
Treatment of cervical cancer
Surgical methods
The extent of surgical intervention directly depends on the extent of the cancer. Modern gynecological oncology strives to perform organ-preserving surgeries in the early stages. The following may be performed:
- Cervical conization. A minimally invasive procedure during which a cone-shaped fragment of the cervix is excised, including the cervical canal. It is used both for diagnostic purposes and as a standalone treatment for young women with preinvasive cancer and microinvasive carcinoma. It allows for the preservation of reproductive function.
- Tracheectomy. A complex organ-preserving procedure involving the removal of the cervix, parametrium, and upper vagina with the placement of a circular suture at the internal os. The uterine body is preserved and fixed in the pelvis. This method is indicated for stage IA2 and some stages IB1 in patients planning a pregnancy.
- Hysterectomy, or complete removal of the uterus. Standard surgical procedure for invasive cancer. Possible surgical options: simple – removal of the uterus and cervix; extended, or Wertheim-Meigs procedure – removal of the uterus and cervix, the upper third of the vagina, parametrium, pelvic tissue, and lymph nodes.
Radiation Therapy
Radiotherapy is a highly effective method that can be used either alone, for example, when surgery is contraindicated, or in combination with surgery and chemotherapy.
Two main forms of radiation are used:
- External beam radiation therapy. The radiation source is placed outside the patient's body. Modern techniques, such as IMRT (tomotherapy) and VMAT (volume-modulated arc therapy), allow for highly precise delivery of maximum doses to the target while minimizing impact on surrounding healthy organs.
- Intracavitary radiation therapy (brachytherapy). During the procedure, a radioactive source is inserted directly into the uterine cavity and vagina in close proximity to the tumor. This provides a powerful localized effect on the tumor.
The most effective treatment for locally advanced cancer is chemoradiation therapy—concurrent radiation and chemotherapy. This significantly increases tumor radiosensitivity and improves long-term outcomes.
Chemotherapy
The use of cytotoxic pharmacological agents solves several problems depending on the clinical situation:
- Chemoradiation therapy uses moderate doses of drugs to sensitize tumor tissue to radiation.
- Several courses of chemotherapy can be administered before surgery to reduce the volume of the primary tumor.
- In metastatic or recurrent disease, systemic polychemotherapy becomes the primary method of palliative treatment, aimed at slowing disease progression, reducing symptoms, and prolonging life.
Rehabilitation measures
A comprehensive rehabilitation program begins immediately after completion of the main course of therapy. It is aimed at minimizing its consequences and returning you to a full life.
- Combating physical complications. This includes lymphedema therapy through specialized massage and compression hosiery, correction of premature menopause, and selection of non-hormonal therapy for urogenital disorders, as well as treatment of possible bladder and bowel dysfunction.
- Psychological support. Working with a psychologist helps overcome anxiety and fear of relapse, accept body changes, and improve quality of life.
- Dynamic monitoring. Lifelong monitoring includes regular gynecological examinations, Pap tests, HPV testing, ultrasound, and CT scans as indicated. Its goal is the timely detection and treatment of possible late complications of therapy and relapses.
Frequently asked questions from patients
Is cervical cancer hereditary?
Can I have children after successful treatment?
How painful is a biopsy?
Does dysplasia need to be treated?
What should you do if the disease returns?
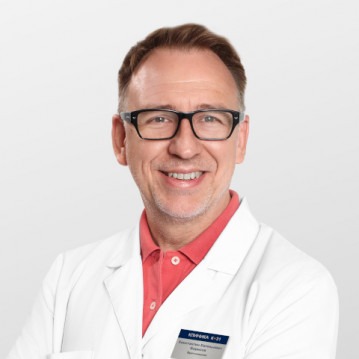
Our doctors

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
News
What do we treat
Price










































































General information about the pathology
Cervical cancer, also known as cervical cancer, develops from abnormal changes in the cells of the cervical mucosa. Anatomically, this area connects the lower part of the uterus to the vagina. One of the characteristics of this area is the so-called transformation zone, or the area where glandular epithelial cells meet the stratified squamous epithelial cells of the vaginal portion of the cervix. It is in this zone that, in the vast majority of cases, the pathological process begins—the uncontrolled division of atypical cells, forming a neoplasm.
The vast majority of cases—over 95%—are directly linked to the persistence, or long-term survival, of highly oncogenic types of human papillomavirus (HPV), primarily types 16 and 18. HPV is a fairly common sexually transmitted infection, but the immune system often clears it on its own. However, with prolonged viral presence, its DNA can integrate into the cell genome, causing uncontrolled cell division and malignant transformation. This process is slow. On average, 10-15 years pass from infection and the appearance of early changes (dysplasia or cervical intraepithelial neoplasia) to the development of cancer.
According to the WHO, cervical cancer is the fourth most common cancer in women. This statistic underscores the social significance of the problem. Crucially, the disease can be prevented and managed, ensuring a favorable prognosis. The long precancerous period provides a unique window of opportunity for effective diagnosis and intervention.
The current strategy for combating cervical cancer is based on two key areas: primary prevention through HPV vaccination and secondary prevention through regular screening.