Cervical biopsy
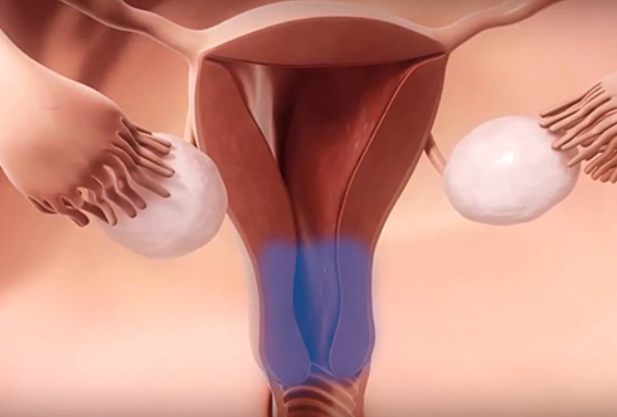
A diagnostic procedure called a cervical biopsy allows you to identify possible pathological changes in the tissue at an early stage. It is widely used in gynecology and involves taking a small piece of tissue (biopsy) for histological examination. This method helps the doctor determine the presence of unhealthy cells and decide on further treatment.

specialists

equipment

treatment
Indications and contraindications
Indications for cervical biopsy
The doctor prescribes a cervical cell analysis in cases such as:
- Suspicion of tissue changes of various nature
- Positive cytological smear results
- Detection of pathological areas during colposcopy
- High risk of having cancer
Diagnostic manipulation is often prescribed in the presence of chronic inflammation, cervical erosion or other abnormalities that require clarification of the diagnosis.
Contraindications
Despite the high information content, the analysis of cervical cells has its limitations. Donating tissue in this way is most often prohibited when:
- Pregnancy
- Presence of acute inflammatory processes
- Bleeding disorders
Before conducting the study, the doctor must prescribe additional tests to eliminate possible risks.
Answers to popular questions
K+31 doctors gave answers to common questions.
Can a biopsy be performed during pregnancy?
Tissue diagnosis of the cervix during pregnancy is possible, but only under strict medical indications, for example, if there is a suspicion of cancer
How long does it take to wait for biopsy results?
The waiting time for results depends on the workload of the laboratory. Typically, a histological examination takes from 5 to 10 working days. I recommend discussing the exact timing with a clinic representative immediately after the procedure.
Can I work or exercise after a biopsy?
Light work is possible the next day, but physical activity, especially intense training, should be avoided for at least a week. This is important to prevent bleeding and infection.
Does the biopsy method depend on the patient's age?
The age of the patient really plays a role when choosing a method. For example, for women of reproductive age, we try to use less invasive methods, such as radiofrequency cell analysis, to minimize the risk of scarring. For postmenopausal patients, when tissue elasticity is lower, other methods are suitable
Will a biopsy affect my chances of getting pregnant in the future?
In most cases, cell testing does not affect your ability to get pregnant. The exception is complex cases with the need to excise a large amount of tissue, which can affect the elasticity of the cervix. Such situations are extremely rare

This award is given to clinics with the highest ratings according to user ratings, a large number of requests from this site, and in the absence of critical violations.

This award is given to clinics with the highest ratings according to user ratings. It means that the place is known, loved, and definitely worth visiting.

The ProDoctors portal collected 500 thousand reviews, compiled a rating of doctors based on them and awarded the best. We are proud that our doctors are among those awarded.
Make an appointment at a convenient time on the nearest date
Price
Other services























































What is a cervical biopsy?
One of the modern diagnostic methods in gynecology is an effective procedure - cervical biopsy, every woman should know what it is and how it is performed. The manipulation itself involves pinching off (or cutting off) a symbolic section of tissue from the cervix for laboratory study and identification of abnormalities.
Taking a cervical biopsy is a procedure in which a doctor, using special instruments, takes a tissue sample for diagnosis. The main goal of the study is to study the structure of cells under a microscope to identify abnormalities.
You can donate tissue for research in various ways, depending on the specific clinical situation:
A cervical biopsy can be performed under anesthesia if a large volume of material is required, or without it if a small area of tissue is needed.