What is the cornea?
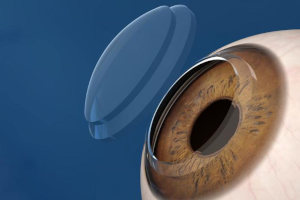
The cornea is the outer transparent convex layer of the eyeball. The maximum thickness of the cornea does not exceed 1.2 mm. The cornea is necessary for clear vision, since it is part of the light-refractive system of the eye, it also performs a protective function, covering the deeper parts of the organ of vision.
The transparency of the cornea is due to the absence of blood vessels; outside, moisture is maintained with the help of lacrimal fluid, which moistens the surface when blinking, from the inside - with moisture from the anterior chamber of the eye.
What are the pathologies of the cornea when surgery is required?
There are two types of pathological processes in which the cornea partially or completely loses its functions:
- Thinning. It cannot fully refract light - the patient's vision deteriorates.
- Appearance of opaque elements. The perception of surrounding objects, clarity of vision is disturbed.
When diagnosing irreversible changes, in order to restore vision, keratoplasty is performed - transplantation of the donor cornea. With the help of which the damaged or thinned area of the transparent layer of the eye is replaced. It is suitable for patients with pathological conditions of the cornea and for people who want to restore the eye after injuries.
Indications for keratoplasty
Corneal transplantation may be a treatment option for eye conditions such as:
- Post-traumatic and postoperative cicatricial changes. After violation of the integrity of the cornea, there is a sharp swelling of the tissues, an influx of leukocytes, and the growth of blood vessels begins in this place. As a result, after a rapidly flowing inflammation, scars form. They are represented by coarse connective tissue, which cannot perform the functions of the cornea. The surface of the eye becomes cloudy, vision is impaired.
- Avascular opaque areas, another name is walleye. They are formed as a result of inflammatory pathologies, ulcers and burns, when connective tissue replaces part of the cornea. Visual acuity decreases, a whitish spot clearly appears on the eye.
- Thinning of the cornea with its subsequent protrusion - keratoconus or keratoglobus. Dystrophic processes are accompanied by a deterioration in vision, a change in the shape of the eye - it protrudes forward in the form of a cone or hemisphere.
Changes in the cornea can lead to its complete clouding and blindness. Keratoplasty partially or completely restores vision in such cases. The cornea has no vessels, so it takes root well. Therefore, if you follow the doctor's recommendations for recovery after surgery, complications can be excluded.
Contraindications for keratoplasty
Absolute contraindications:
- Inflammatory diseases of the eyeball;
- Belmo, in which the blood vessels are located;
- Obstruction of the lacrimal canal;
- Increased IOP;
- The presence of pathologies in which the risk of graft rejection is high.
Relative contraindications:
- CVD diseases (relative contraindication);
- Lung diseases;
- The presence in the body of infectious foci in the form of caries, otitis or sinusitis, which must be cured before corneal keratoplasty.
Types of corneal replacement surgery
- By volume of intervention - total, subtotal, local.
- According to the layers that replace - through, layered back, layered front.