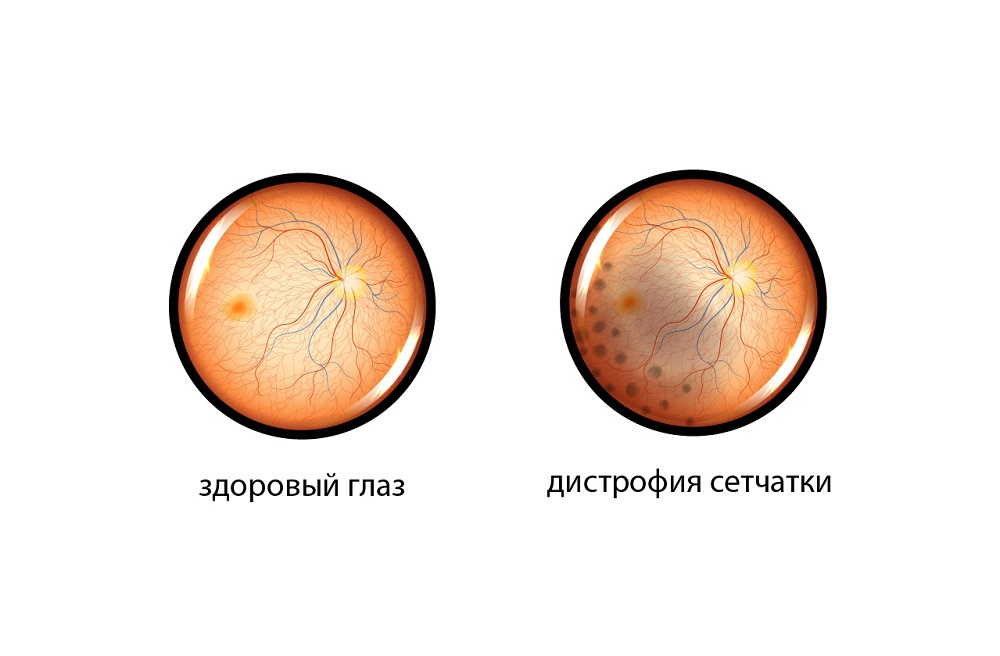
Retinal dystrophy is a condition accompanied by a violation of its nutrition. Metabolic processes are disrupted at the cell level, then functional and structural changes are noted.
Diseases and conditions leading to retinal dystrophy:
- Diabetes.
- Arterial hypertension.
- High myopia.
- Common atherosclerosis.
- Traumatic brain injury.
- Eye damage.
- Consequences of infectious and viral diseases.
Allocate central retinal dystrophy, in which changes develop in the macula - the exit point of the optic nerve. This area is responsible for visual acuity and perception of small objects. In the early stages, the disease may not manifest itself in any way. Later, vision deteriorates, dark spots appear in front of the eyes and difficulties in focusing on small details.
The second type is peripheral dystrophy. The foci of pathology are located outside the macula, which is why they do not manifest themselves in any way. Peripheral dystrophy is dangerous with retinal detachment, therefore, laser coagulation is indicated.
An ophthalmologist deals with the diagnosis of pathology. In the K+31 clinic, it is possible to undergo examination and treatment using modern equipment that allows you to accurately identify and successfully eliminate degenerative changes in the retina.
Indications
Conditions in which the operation is required: retinal detachment or rupture, lattice thinning, dystrophy of the "snail trace" type, the presence of blood clots in the vessels of the eye, diabetic changes, macular edema.
Contraindications
The operation is not performed in the presence of hemorrhage in the eye cavity, cataracts, formation of gross gliosis (gliosis is an overgrowth of connective tissue that can grow into the vitreous body, disrupting the functioning of the organ of vision). Laser correction can be performed after elimination of the pathology.


