The information presented will help you understand modern assisted reproductive technologies (ART) using such a popular technique as in vitro fertilization (IVF). With the help of ART, many couples with reproductive disorders managed to give birth to healthy children.
Natural conception.
To understand the essence of ART, it is important to understand how natural conception occurs. For the successful fertilization of an egg, the following key conditions are necessary: fertile sperm of the partner, full ovulation and patent fallopian tubes in the partner.
In the ovaries of a woman of childbearing age, there are many rudiments of follicles that are waiting for their turn to mature, and each cycle, either in the left or in the right ovary, usually one dominant follicle stands out among them.
Approximately in the middle of the menstrual cycle, under the influence of hormones, ovulation occurs, which is preceded by the rupture of the follicle membranes and the release of a full-fledged egg from it. During ovulation, the ovum leaves the ovary into the abdominal cavity, and then enters the fallopian tube located near it, the inner layer of which is lined with villi. These villi of the fallopian tube tightly capture the egg and allow it to wait for about a day for a sperm to fertilize it.
During intercourse, up to 500 million sperm penetrate into the female vagina during ejaculation. Full and motile sperm cells live in the female body for about 7 days, which means that intercourse does not have to be strictly on the day of ovulation. Thanks to a special enzyme, sperm cells dissolve the cervical mucus of the cervix and penetrate into the woman's reproductive organs. Only one of the several million sperm that have penetrated deep into the fallopian tube manages to rupture the membrane of the egg and then fertilize it. As a result of the fusion of a sperm with an egg, a zygote is formed - the initial stage of pregnancy development (Figure 1).
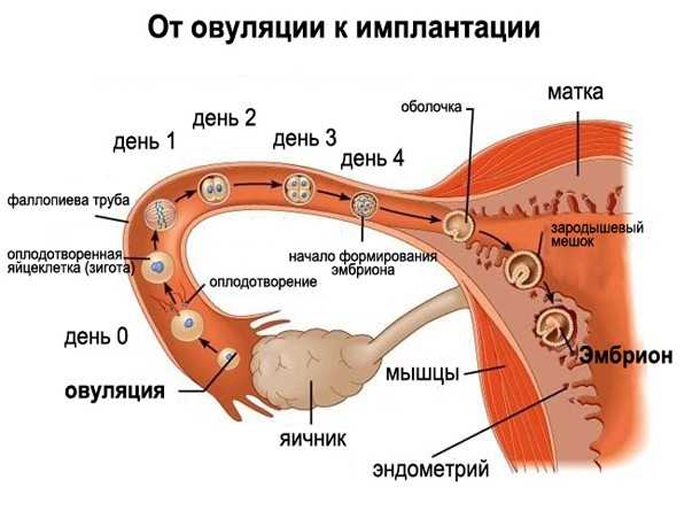
Figure 1. The process of implantation and ovulation.
In Vitro Fertilization (IVF).
Modern reproductive technologies for the treatment of infertility offer many infertile couples in vitro fertilization, in which the process of conception takes place outside the female body - in a test tube.
Usually, one or two embryos are transferred into the woman's uterine cavity, and the remaining embryos are cryopreserved for possible future use. Initially, IVF was used to treat women with obstructed patency or absence of fallopian tubes. Today this method is used to treat many severe forms of infertility, including male factors.
The IVF cycle includes the following stages: stimulation of ovarian function, transvaginal puncture of the ovaries for oocyte collection, fertilization, embryo culture and embryo transfer into the uterine cavity. We will describe all these stages in more detail in the following subsections.
Stimulation of ovarian function.
During the stimulation of ovarian function, hormonal drugs are used, as a result of which not one ovum matures in the female body, as in the natural cycle, but several at once (Figure 2).
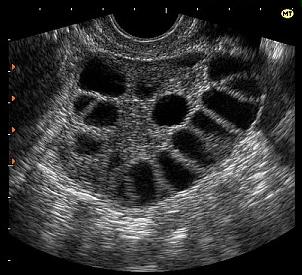
Figure 2. Stimulation of ovarian function.
Ovarian stimulation drugs
Human menopausal gonadotropin (MHG)
Follicle-stimulating hormone (FSH)
Luteinizing hormone (LH) (used in combination with FSH)
Chorionic gonadotropic hormone (CHG)
Clomiphene citrate
Letrozole
Drugs to prevent premature ovulation
Gonadotropin-releasing hormone (GHH)
Treatment with analogs of SHG
The choice of the drug and the stimulation protocol for a particular patient is made by the reproductive physician, based on many factors. Ovulation is stimulated for an average of 10 days, during which ultrasound monitoring of follicle maturation and growth is carried out. When the follicles reach a certain size, drugs are used to stimulate the final stage of oocyte maturation so that the oocytes become fertile. The eggs are removed before ovulation begins, usually 34 to 36 hours after the injection is given.
With the maturation of a large number of follicles in order to prevent the development of ovarian hyperstimulation syndrome (OHSS), the IVF cycle can be segmented. That is, all the obtained embryos are cryopreserved and transferred in an unstimulated cycle in the "cryo transfer" program.
Transvaginal ovarian puncture for oocyte collection.
Transvaginal ovarian puncture is performed by aspiration of follicular fluid through a thin aspiration needle under ultrasound guidance.
Follicular puncture is performed under short-term intravenous (10-20 minutes) anesthesia. A transvaginal ultrasound probe is located in the vagina, with which mature follicles are visualized, and a thin needle is inserted into the follicles through the vaginal wall. Follicular puncture is a minor surgical operation and does not require hospitalization (Figure 3).
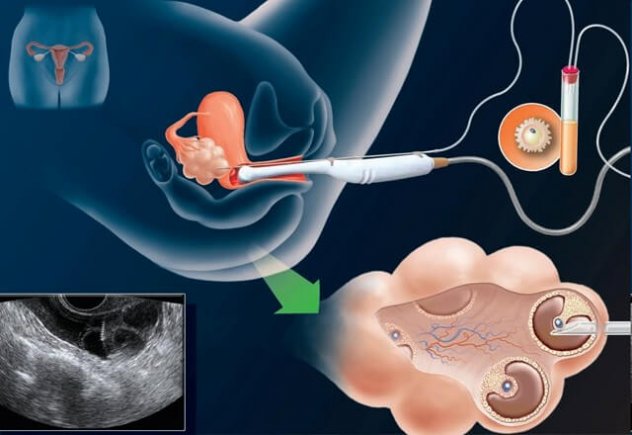
Figure 3. Transvaginal ovarian puncture in the IVF program
Embryo cultivation.
After the eggs are retrieved, they are examined in the laboratory for maturity and quality. Mature eggs (Figure 4) are placed in a special environment and transferred to an incubator to await their fertilization with sperm.
Simultaneously with the puncture of the follicles, the man donates sperm, which will be used to fertilize the eggs. Then the prepared sperm is added to the eggs, placed in a special nutrient medium, and left in the incubator, where fertilization takes place.
After 16-18 hours, under a microscope, the quality of fertilization, the number of pronuclei (should be 2) and their morphology are assessed (Figure 4). With further cultivation of embryos, after another 24 hours, the quality of cleavage is assessed (at this stage, embryos usually reach the 4-6 blastomeric stage). After another 24 hours of cultivation, the embryos reach the 8-10 cell stage (Figure 5). At this stage, the embryos can be transferred into the patient's uterine cavity. However, a more favorable prognostic sign is further cultivation of embryos to the blastocyst stage (5-day-old embryos) (Figure 5).
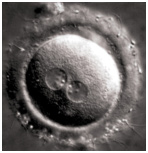 Figure 4. Zygote with two pronuclei
Figure 4. Zygote with two pronuclei
 Figure 5. Eight-cell embryo
Figure 5. Eight-cell embryo
 Figure 6. Blastocyst
Figure 6. Blastocyst
Transfer of embryos into the uterine cavity.
The next step in the IVF program is the transfer of the embryo into the uterine cavity. This procedure is painless and performed without anesthesia. The doctor opens the cervix using a speculum. One or two embryos are placed in a special tube (catheter) with a syringe at the end. The doctor gently inserts the end of the catheter through the cervix and places the embryo medium into the uterine cavity (Figure 7).
Since each embryo has an equal probability of implantation and development, the number of embryos to transfer must be determined for each patient individually. Recently, in well-equipped ART clinics, there has been a tendency to transfer one embryo into the uterine cavity in order to minimize the possibility of multiple pregnancies and associated complications.

Figure 7. Transfer of embryos into the uterine cavity
Immediately before embryo transfer, so-called "assisted laser hatching" is often performed - a micromanipulative procedure in which a hole is made in the extracellular membrane of the oocyte to facilitate the process of embryo attachment to the uterine wall. Assisted hatching can be used to help older women or couples who have had unsuccessful IVF attempts.
Preimplantation genetic diagnosis (PGD) is used to detect hereditary diseases. During the procedure, an embryo biopsy is performed on the 5th day of cultivation. Embryos that do not have disease-related genes are chosen for transplant into the uterus. Some couples, especially those who carry genetic diseases, find embryo screening a beneficial procedure to reduce the risk of having a baby with a disability. In addition, this diagnosis is extremely effective for couples with a history of unsuccessful IVF attempts.
Cryopreservation.
The embryos remaining after the transfer can be cryopreserved (frozen) for future transfer. Cryopreservation simplifies future ART cycles, making them less expensive and less laborious than the initial IVF cycle, since the woman does not need restimulation of ovarian function and transvaginal puncture. Once frozen, embryos can be stored for a long period of time. To date, the effectiveness of the IVF program in cryoprotocol cycles does not differ from that of the embryo transfer in a fresh cycle. Cryopreservation is usually carried out on the 5th, sometimes 6th day of cultivation.
It is also worth noting that more and more ART centers cryopreserve oocytes (eggs) before fertilization to preserve the genetic material of women. This method is most often used for young women who are about to undergo treatment or procedures that may affect their future fertility, for example, when prescribing chemotherapy for cancer. In addition, this procedure is carried out for women who do not plan to implement their reproductive function in the near future.
Donor programs.
IVF can be performed using your own eggs and sperm, or using donor genetic material. A female ovum carries a set of female chromosomes, just as a sperm cell carries a set of male chromosomes. A couple can choose a donor if there is a problem with their own sperm or eggs, or if they have genetic abnormalities that can be passed on to the child. The donor can be either anonymous or non-anonymous. Sperm donors and egg donors undergo medical and genetic testing. Donor sperm is frozen for 6 months and repeated tests for infectious diseases. Sperm are allowed for use if all tests are negative.
Donated eggs are the only option for some women to have children of their own. The circumstances for which a woman is forced to resort to donor eggs may be different. The main reason for a woman's lack of eggs is premature ovarian depletion. That is, menopause in this case occurs in a woman at a young age, and if she did not have time to realize her reproductive function before that time, the only way out for her is to resort to a donor egg taken from a young healthy woman. In other situations, the cause is related to previously performed operations on the ovaries, for example, in cases where the ovaries had to be removed due to the occurrence of a tumor. After recovery, these women will also not be able to have children of their own, unless they use donated eggs from another woman. There are also certain circumstances in which a woman cannot have children due to certain genetic abnormalities.
Thus, when a woman wants to become pregnant, but she does not have her own eggs, she can either adopt a child or resort to a donor program. Thanks to the donor program, she gets the opportunity to fully experience the joy of motherhood, including the process of pregnancy and childbirth. In this case, the child will carry the genetic information of the father and the oocyte donor.
In some cases, when both partners - both the man and the woman - are infertile, both donor sperm and donor egg are used, but in such situations it is more expedient to use donor embryos.
Surrogacy.
Surrogacy is one of the ART methods that is used in cases when a woman, due to health reasons, cannot bear and give birth to a child. Thirty years ago, the only way out in such a situation was adoption. Currently, infertility can be successfully overcome even in the absence of a uterus in a woman or with an anomaly of its development.
The essence of the program is that a surrogate mother bears a child who has no genetic relationship with her: the embryo is obtained using IVF, where the biological mother's eggs are fertilized with the biological father's sperm. After that, the embryo is transferred to the surrogate mother into the uterine cavity, which, according to the contract, undertakes to transfer the child to the mother and father after birth. It is they who will be registered as legal parents of the baby in the registry office.
The surrogacy program is carried out according to a certain algorithm. First you need to find a surrogate mother. This issue must be approached with all seriousness. Each surrogate mother must undergo a thorough examination, she must be completely healthy, mentally normal, psychologically adequate and be able to participate in the program in the near future.
Surrogacy in Russia is absolutely legal and regulated on the basis of current legislation. Couples usually seek help from specialized centers that have their own database of surveyed women, which fully comply with the requirements of the Ministry of Health of the Russian Federation and are ready to immediately enter the program. An agreement is concluded between the substitute mother and the biological parents, which contains the obligations of the parties and is drawn up by lawyers in relation to each specific situation. Usually, specialists from IVF clinics solve all issues related to the legal support of the procedure, up to the moment the child is registered with the registry office.
The main risks of ART.
In some cases, stimulation of ovulation, which is carried out under the influence of hormones introduced from the outside, in order to obtain several eggs in one menstrual cycle, entails the risk of developing ovarian hyperstimulation syndrome. The cause of OHSS is the development of a large number of follicles (more than 15), which leads to high ovarian activity. In this case, the vascular permeability is impaired and the fluid from the vessels begins to flow first into the pelvic cavity, and then into the abdominal cavity. As a result of the accumulation of fluid in the abdominal and pleural cavity, the patient may experience a feeling of "fullness", nausea, vomiting, lack of appetite. About 30% of patients undergoing ovarian stimulation have mild OHSS, which does not require much effort to overcome. With moderate hyperstimulation syndrome, patients accumulate fluid in the abdominal cavity and pain in the gastrointestinal tract. These women need supervision, but outpatient treatment is usually sufficient in such situations. Gradually, the condition of such patients has a positive trend without additional intervention, but in case of pregnancy, the improvement can be delayed for several weeks. In 1-2% of patients, severe OHSS develops, characterized by fluid accumulation in the abdominal and pleural cavities, electrolyte imbalance, and increased blood clotting. Patients with severe ovarian hyperstimulation require hospitalization until their condition improves, which may take several weeks.
With ART, the likelihood of multiple pregnancy increases when more than one embryo is transferred. While twins are considered lucky by some, there are many problems associated with multiple pregnancies. Complications become more serious and common with three or more fetuses. The risk of premature birth in multiple pregnancies is high, and premature babies require long-term and intensive care.
Ovarian torsion is another risk during ART. As a rule, after the stimulation of superovulation for some time, the ovaries remain enlarged in size by 1.5-2 times. This is due to the fact that at the site of the aspirated follicles "yellow bodies" are formed, which support pregnancy up to 10-12 weeks. The enlarged ovaries become extremely mobile, and can, in rare cases, twist on their ligaments. Torsion is manifested by sharp pain, the intensity of which is constantly increasing. In such situations, a laparoscopic operation with the "unwinding" of the ovary is indicated, and if irreversible changes have occurred in the ovary, then the removal of part or all of the ovary.
After embryo transfer, patients should carefully monitor their condition. In order to prevent the development of these serious complications, it is recommended to limit physical activity, exclude sexual activity during the first two months of pregnancy after IVF.
Although it has previously been suggested that the use of stimulant drugs may increase the risk of ovarian cancer, numerous recent studies have not found any association between drugs to stimulate superovulation and cancer of the ovary or other organs.
Bleeding in the first trimester of pregnancy can signal a possible miscarriage or ectopic pregnancy. If bleeding or pain occurs (up to 13 weeks), a medical examination should be done to determine the cause. As a rule, bleeding in the early stages most often occurs in women undergoing IVF and PMHT.The likelihood of an ectopic pregnancy when using ART is about 5% of cases. There is no data on whether the risks of having children with disabilities are increased with the use of IVF. Most studies do not show an increased risk, while others suggest it exists.
Assisted reproductive technologies involve significant physical, financial and emotional obligations on the part of a couple. Psychological stress is a common problem. Treatment is time consuming and costly. Patients have high expectations, and given that the success of the IVF program is not 100%, failure is still possible. Therefore, we advise prospective parents to consider going through psychological counseling as an additional means of support and stress management. Many ART clinics employ mental health professionals to help couples cope with regret, pressure, or anxiety related to infertility or its treatment.
Preparation before IVF.
Preparation before IVF includes an assessment of the health of future parents, as well as preparation of a woman's body for carrying a pregnancy. Examination of a married couple before planning a pregnancy is necessary and begins well in advance.
In some cases, a married couple needs a consultation with a geneticist to determine the risk of having a child with a hereditary pathology. Absolute indications for medical genetic counseling are: hereditary diseases or developmental defects in the family; consanguineous marriage; age over 35, spontaneous miscarriages, miscarriage, intrauterine fetal death, history of stillbirth.
With favorable results of the study of the state of health, future parents can prepare for conception. First of all, you need to give up bad habits, observe the daily routine, have moderate physical activity, fully sleep and rest, avoid negative emotions and stress. Parents-to-be should have a balanced and high-quality diet, especially during the period of pregravid preparation.
The use of various multivitamin preparations for pregnant women is best discussed with your doctor. Vitamin overdose is just as dangerous as vitamin deficiency. Therefore, they need to be taken only after consulting a doctor and according to his appointment.
Preparation before IVF for women : during a consultation with a reproductive specialist, the condition of the female reproductive system is assessed by examination, ultrasound, hormonal examination, assessment of the ovarian reserve, examination for sexually transmitted infections. If necessary, a pipel biopsy of the endometrium, hysteroscopy, separate diagnostic curettage of the endometrium and cervical canal, laparoscopy are performed. Before carrying out an IVF program, it is necessary to consult a therapist to identify and eliminate somatic pathology, which is a contraindication for carrying a pregnancy. If necessary, the patient is referred to consultations of narrower specialists - endocrinologist, gastroenterologist, nephrologist, cardiologist, etc.
Preparation before IVF for men : before the IVF program, a man undergoes an examination by an andrologist to assess the state of the male reproductive system, which includes a spermogram, ultrasound, examination for sexually transmitted infections. When interpreting the spermogram result, such indicators as high mobility (category a + b) and the number of sperm with normal head morphology, tail neck according to strict criteria are important. In case of serious deviations of the spermogram from the norm, a more complete examination and adequate preparation for the IVF program are necessary. It is important to identify and eliminate harmful effects on the body of the future father and, as a result, on spermatogenesis (alcohol, smoking, medicines, infections, household and occupational hazards, physical inactivity, and other factors). It is very important to stop visiting baths, saunas, and taking hot baths.When to end treatment.
Studies show that when using the IVF program, the chances of getting pregnant in each of the four IVF cycles are the same for a couple. With subsequent cycles, the likelihood of a positive result decreases. However, given the current expanding capabilities of ART, repeat IVF programs are more likely to be successful. As the couple's management tactics will be adjusted based on previous results, the doctor will have more confidence in a successful outcome.
Of course, there is no generally accepted maximum number of acceptable IVF attempts. Everything will depend on you and the decision of your doctor, who, like no one else, will see the whole picture and the situation. When deciding on the possibility of carrying out the next fertilization attempt, the doctor is guided by the results of past procedures and analyzes, the individual characteristics of the patient's body, her psychological state, age and other significant parameters.
Conclusion.
Today, the decision to search for infertility treatment is relevant due to the availability of ART. With patience, a positive attitude, and an appropriate treatment program, most infertile couples end up with a high chance of having a healthy child.

