SARS-CoV-2 has taken a firm place in our lives. It is already obvious that it will not disappear like the chicken flu, flashing terrible news on the pages of newspapers. With this new type of threat to life and health, you need to learn to live. Observe hygiene rules, get vaccinated, not forgetting that the dangerous COVID pandemic is always nearby.
Why do some people get SARS-CoV-2 on contact, while others do not
To effectively combat the SARS virus, it is necessary to understand the mechanism of its spread, how the infection occurs. It is already known that many people, after prolonged repeated contact with infected people, do not get sick themselves. Why it happens? Obviously, only a person with a strong immune system may not have any clinical symptoms after direct contact with the pathogen.
The infectious process proceeds in different ways, depending on many factors, as a result, the mechanisms and timing of the formation of anti-SARS antibodies by B-lymphocytes are different. This is important, but it's not just antibodies that matter. Cellular immunity, mediated by the cells of the immune system, is also important, but antibodies are not involved in this process. The humoral immune response to pathogenic flora is important, which indirectly depends on the antibodies in the blood.
The cellular link (primarily the T-cell) plays a significant role in the stability, resistance of the immune system. Its function is simplified to informational:
- The virus needs to be identified.
- Transfer melon to other links about the appearance of foreign substances (antigen).
- Destroy SARS-CoV-2.
- Save information about its features in memory.
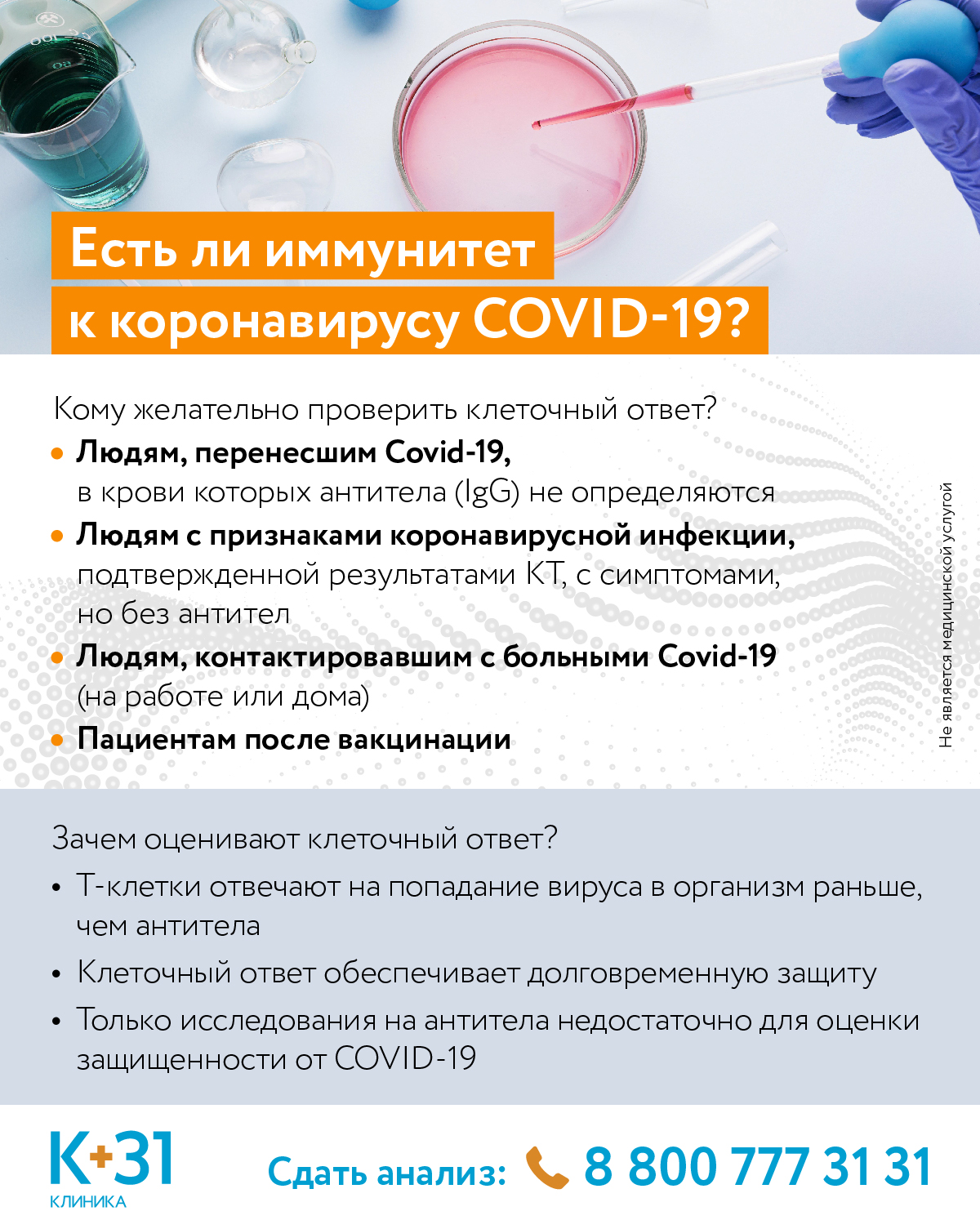
In some people, presumably with a low amount of the pathogen that has entered the body, the T-cell link removes the virus from the body with a low activity of the link responsible for the formation of antibodies. Since the B-cell link is practically not involved (not activated), traditional laboratory methods do not allow diagnosing pathology. T-cell immunity tests are not performed. There are also no clinical symptoms with a small volume of the virus, since the infectious process does not develop. Therefore, the attending physician often cannot even make a diagnosis.
It is already known that natural infection with a small amount of the virus, which the body manages to defeat, strengthens T-cell immunity, despite the lack of antibody activity. The risk of re-infection with SARS-CoV-2 is reduced. However, how stable protection the T-cell link provides, and how long it lasts, remains a mystery for the attending physicians.
T-cell immune response to coronavirus
But it is already known that in the majority of patients who are faced with SARS-CoV-2, a persistent immune response of the T-cell link is formed. And those who have never met the pathogen have T-lymphocytes that react to the virus. Various forms of coronaviruses are likely to be widespread in the human population. The response of the T-cell link to them is precisely what provides increased immunity to the virus that causes COVID.
Thus, the low susceptibility to SARS-CoV-2 is highly likely due to immunological memory. Those. previous contacts with similar viruses help develop the body's immunity to coronavirus. If earlier T cells came into contact with similar antigens, the body's resistance to SARS-CoV-2 is much higher.
This conclusion is difficult to verify using mass laboratory anti-SARS studies. This is a very long process, and so far it is not nearing completion. However, the data already obtained in research laboratories inspire optimism.
A topical alternative - antibody tests
So far, the test for T-cell immunity is not carried out, and the attending physicians in their practical work focus on the detection of antibodies. It is their study that makes it possible to determine the body's resistance to SARS-CoV-2 when a large amount of the agent enters the body. There are two most popular and effective anti-SARS areas:
- Antibodies of class G to nucleocapsid protein (coronavirus). Resistant to the SARS-CoV-2 protein, aka Anti-SARS-CoV-2 nucleocapsid protein igg; SARS-CoV-2 anti-nucleocapsid protein IgG, etc.
- Igm antibodies. Also common names are: antibodies to coronavirus S (spike); qualitative analysis of anti-SARS; class M immunoglobulins to the coronavirus protein, etc.
This information will be useful to everyone who is conscious of their health: both healthy and already sick with COVID. The presence of IgM indicates the initial stage of contact with the pathogen, up to 2 weeks. IgG (G) is usually detected at 3-4 weeks.